Playlist
Show Playlist
Hide Playlist
Hemolytic-Uremic Syndrome (HUS): Signs and Symptoms
-
Slides InfectiousDiarrhea InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
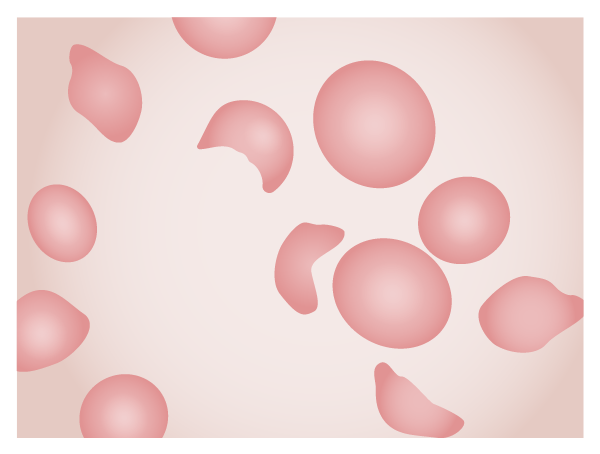
00:00 An unusual disorder but an important disorder to mention is something called the hemolytic- uremic syndrome and this is caused by one of the toxin-producing E. coli, the Shiga toxin- producing E. coli or STEC and the most common of the E. coli to do that is an organism E. coli O157:H7 and this is the kind of minute point that you may want to study up on for step exams. 00:41 The incidence is, however, low. It's 5 to 10% of those who get infected with E. coli O157:H7 and some other E. coli can possess that Shiga toxin and they cause exactly the same disease. 01:00 Shiga toxin producing Escherichia coli (STEC), called typical HUS, is the most common cause of HUS Typical HUS comprises 90% to 95% of HUS cases, and commonly arises from consuming contaminated food or drink and through person-to-person contact. 01:20 You might also recognize since it's Shiga toxin that some Shigella can also cause this disease and it turns out that Shiga toxin 2 is the most important and that's possessed by Shigella dysenteriae. So what's the pathology of this disorder? Well, what happens is there is deposition of complement along the endothelium of the blood stream and especially intimal hyperplasia of the small renal arteries. I think you can see where we're going with this uremia-like syndrome. You get occlusion of blood vessels fibrin deposits and along with this a hemorrhagic colitis and not only that but there's a blood dyscrasia as well, a microangiopathic hemolytic anemia. What that means is that with this endothelial problem in all the clots as blood passes through these abnormal blood vessels, the shearing force increases and so there are schistocytes, helmet cells and other types of red cell distraction that you can see on a peripheral blood film. So the way it presents is usually in infancy or early childhood and on the first day of this the patient will have abdominal cramps and non-bloody diarrhea but by day 2 they start having high volume bloody stools and interestingly enough you don't usually find that much in the way of white blood cells in the stool. Many of the patients have severe nausea and vomiting and test of renal function are markedly abnormal, severe renal failure. 03:19 Interestingly enough, this usually resolves completely. They will have this microangiopathic hemolytic anemia. High fever is not characteristic and as I mention very few fecal white cells and thankfully it has a very good prognosis. So how do you identify this particular brand of E. coli? Well, E. coli O157:H7, the way they test for it is they use Sorbitol-MacConkey agar. 03:54 Now, first of all MacConkey agar usually has lactose in it, not the sugar sorbitol. So normally MacConkey agar is used to differentiate between lactose-fermenting and non-lactose- fermenting organisms. Well if you use that for this O157:H7, it would be a lactose fermenter but it was discovered that if you substitute sorbitol instead of lactose, no lactose in this MacConkey agar, this organism is sorbitol negative. In other words, it does not turn red and I'm showing you that on the right of a sorbitol negative MacConkey agar to be contrasted with the rest of the E. coli which are easily able to ferment sorbitol and produce a change in the color of the dye. You then have to confirm the serotype that's causing this problem.
About the Lecture
The lecture Hemolytic-Uremic Syndrome (HUS): Signs and Symptoms by John Fisher, MD is from the course Gastrointestinal Infections. It contains the following chapters:
- Hemolytic-Uremic Syndrome – Signs/Symptoms
- Hemolytic-Uremic – Pathology
- Hemolytic-Uremic Syndrome vs. TTP
- E. coli O157-H7 (Identification)
Included Quiz Questions
Which of the following accounts for the majority of cases of hemolytic uremic syndrome in children?
- Shiga toxin-producing Escherichia coli
- H1N1 influenza A
- Drugs
- Streptococcus pneumoniae
- Acute lymphoblastic leukemia
Microangiopathic hemolytic anemia in patients suspected of hemolytic uremic syndrome and anemia can be confirmed with which of the following laboratory findings?
- Large number of schistocytes on blood smear
- High counts of fecal white blood cells.
- Reduced glomerular filtration rate
- Positive stool cultures for shiga toxin-producing Escherichia coli
- Elevated liver enzymes
What is the most likely prognosis of a child with typical hemolytic uremic syndrome?
- Full recovery
- Permanent renal insufficiency
- Death
- Myocarditis
- Bone marrow failure
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excelente muchas gracias me gusto pude encontrar lo que buscaba.