Playlist
Show Playlist
Hide Playlist
Hemolytic-Uremic Syndrome (HUS) in Children
-
Slides HUS Pediatrics.pdf
-
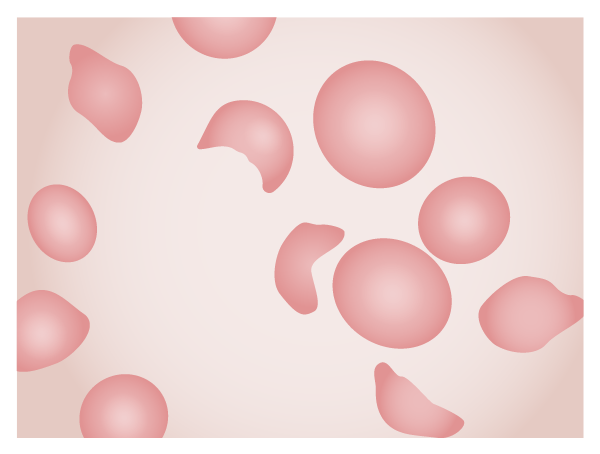
Download Lecture Overview
00:00 In this lecture, we're going to review Hemolytic-Uremic Syndrome in Children. Hemolytic-uremic syndrome is a combination of a few different findings. These patients have a microangiopathic hemolytic anemia. They'll have acute kidney injury and they'll have thrombocytopenia. So, anemia and thrombocytopenia as well as kidney injury. This disease typically happens in children under 5 years of age and it's the most common cause of acute kidney injury in children. If it's preceded by diarrhea, the mortality is fairly low, 4% although those odds are what you would like for your own child. If it's not preceded by diarrhea, the mortality is high, 25%. Hemolytic-uremic syndrome used to be classified into diarrhea positive and diarrhea negative types. But that classification has been replaced by an etiologic classification because diarrhea can be associated with different etiologies. The updated classification of HUS includes acquired and hereditary types. There are several points to highlight in this large classification. 01:20 Note that Shiga toxin-producing E. coli or STEC accounts for 90% of the cases in the US whereas Shigella dysenteriae type 1 is a more common cause in developing countries. 01:35 Streptococcus pneumoniae accounts for 40% of non-STEC cases. Hereditary types are mostly caused by mutations in the genes' coding for complement components or in those coding for proteins involved in the coagulation pathway. We typically see patients getting E. coli 0157 from undercooked meats, unpasteurized milk, unwashed fruit and vegetables or petting zoos. 02:06 We tend to see little outbreaks happen sometimes from petting zoos where that bacteria has become prevalent and patients are perhaps not cleaning their hands appropriately after petting the farm animals. Non-STEC-HUS cases are most often caused by Streptococcus pneumoniae lung infections especially if they're associated with pleural effusions, but this is rare. HIV can also cause non-STEC-HUS. Infectious HUS is typically an illness that starts with bloody diarrhea. So in a large study at the Children's Hospital of Philadelphia, they looked at many decades and they only found a handful of cases, but in those cases it is usually from patients who had complicated pneumonia with pleural effusions. Medications such as cyclosporine or tacrolimus can also cause non-STEC-HUS. Also, HIV can cause the problem and so we might see this in patients with HIV. So, infectious HUS is typically an illness where it starts with a bloody diarrhea. Patients may have vomiting and fever with the acute illness from the usually E. coli 0157. This diarrhea may resolve or it may still be present when the new symptoms occur. And the new symptoms will be an acute onset of lethargy, irritability, and key pallor. These patients will develop oliguria. They're developing oliguria because their kidneys are shutting down. They may have neurologic syndromes present as well such as altered mental status or seizure. The point is that these children can be very sick, 10% of them can go into congestive heart failure. They can have all kinds of substantial problems and we have to watch them very carefully. Here is an example of what a slide might look like if you are to look at the blood of a patient with hemolytic-uremic syndrome. They will have schistocytes or other evidence of a normocytic anemia; however, there will be evidence of the microangiopathic nature of this anemia. Remember, these cells are being viciously split apart inside the blood vessels. Additionally, patients typically have a low platelet level usually between 20,000 to 100,000 platelets. This is because, again, of a consumptive coagulopathy. 04:40 In patients with hemolytic-uremic syndrome, the Coombs test should be negative. This is not an antibody-mediated disease, these cells are being broken apart because it's a microangiopathic state. A urinalysis will show hematuria and proteinuria. Additionally, we may get a chem-7. The chem-7 will show a high BUN and creatinine consistent with intrarenal disease. If it's severe, the patient may have high potassium from renal failure or from cell lysis in combination from renal failure. And because of their hemolysis, patients will have a high LDH and often a high indirect bilirubin and maybe frankly jaundiced. In patients with hemolytic-uremic syndrome, they have a bloody diarrhea caused by E. coli 0157:H7. It may be tempting to give them antibiotics to treat that E. coli and to think that that might prevent the hemolytic-uremic syndrome. On the contrary, it seems that treatment may, in some patients, actually increase risk of HUS. So we do not treat patients with antibiotics in this condition. 05:54 What we will do is treat people symptomatically for their problems. First, we need to be very careful with fluid and electrolyte management. Remember, we're trying to maintain a situation where the child is remaining hydrated and yet in the child there may be some renal failure. 06:12 Also, a high potassium is an emergency because patients may have arrhythmias. So we have to keep an eye on that potassium. Close monitoring of both fluid and electrolytes is absolutely indicated. If patients end up in trouble, we may have to do dialysis to try to control levels of electrolytes and the fluid in the blood. We also want to control their hypertension. We can't let that get out of control and we may provide medications for that purpose. If patients are seizing, we need to control the seizures as well and we'll provide seizure medications. It's important to transfuse children if they are symptomatic and have tachycardia. We usually try to keep them above approximately the level of 7, but do not transfuse platelets. It would be rare for these children to get into a trouble zone say less than 5000 to 10,000 and the platelets almost immediately get consumed. So, you'll just worsen the coagulopathic state. 07:15 In resource rich countries, the mortality rate of HUS is less than 5%, but another 5% of patients have significant sequelae for example stroke or end-stage renal disease and 30-50% of children will show evidence of irreversible renal injury manifesting as hypertension, mild proteinuria, a subclinical decline in glomerular filtration rate, and chronic kidney disease. The mortality rate of HUS in underdeveloped countries remains as high as 72%. However, some patients progressed to end-stage renal disease and may eventually need a transplant. The key thing here is that we have to promote handwashing and safe processing of foods and certainly handwashing when visiting the petting zoo. That's a summary of hemolytic-uremic syndrome. 08:10 Thanks for your attention.
About the Lecture
The lecture Hemolytic-Uremic Syndrome (HUS) in Children by Brian Alverson, MD is from the course Pediatric Nephrology and Urology. It contains the following chapters:
- HUS
- Diarrhea Negative HUS
- HUS – Diagnosis
Included Quiz Questions
Exposure to which of the following is a common cause of HUS in children?
- Farm animals
- Personal pets
- Daycare facility
- Other patients with diarrhea
- Blood transfusions
Which of the following is the most common cause of hemolytic uremic syndrome in children?
- Shiga toxin-producing Escherichia coli
- Cyclosporine
- Pneumococcus
- Systemic lupus erythematosus
- Anti-phospholipid antibody syndrome
Which of the following is true regarding diarrhea-hemolytic uremic syndrome (HUS) and diarrhea-negative HUS?
- Diarrhea-associated HUS is the more common type in children.
- Diarrhea-associated HUS has a higher mortality rate.
- The most common cause of diarrhea-associated HUS in Pneumococcus.
- Diarrhea-negative HUS does not occur during pregnancy.
Which of the following infectious agents is the most common cause of diarrhea-negative HUS?
- Streptoccus pneumoniae
- Escherichia coli
- Staphylococcus aureus
- Salmonella typhi
- Neisseria gonorrhoeae
Which of the following is NOT a complication of diarrhea associated HUS?
- Coombs positive microcytic anemia
- Acute renal failure
- Thrombocytopenia
- Seizures
- Hyperkalemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great explanation of key concepts, classification and management. Makes it much easier to remember.
Thank you very much for a clear, concise summary of this topic.