Playlist
Show Playlist
Hide Playlist
Going from Acute to Chronic Inflammation
-
Slides Acute and Chronic Inflammation Moderate Acute Inflammation.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
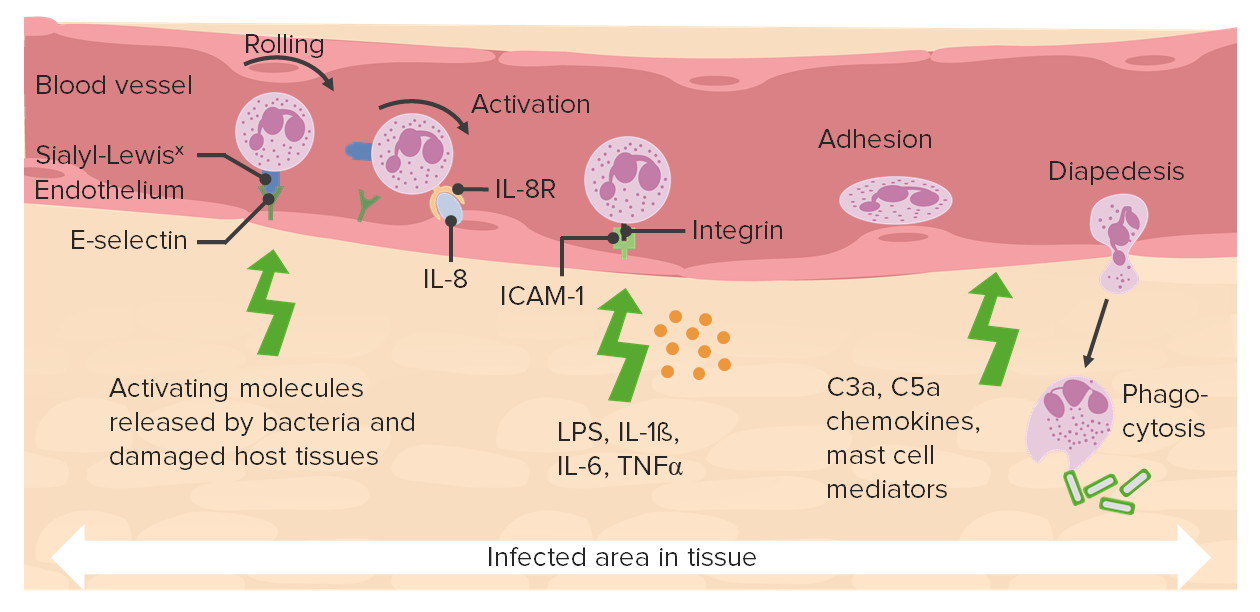
00:01 Let's talk about then, what's going on in the tissue? So those were a bunch of words. 00:05 Let's see a diagram. 00:06 Here we have our blood vessel at the top, and neutrophils have come out. 00:11 Remember, the clock is ticking for them. 00:12 They have 10 hours and they're gonna die. 00:14 They are going after the necrotic tissue and or the area of infection. 00:19 And they will catabolize that using proteases and other things, and we'll get debris. 00:27 At about the same time that we've peaked for our neutrophil extravasation, we're now going to start recruiting monocytes that will turn into mature into macrophages. 00:39 So there will be at certain times in the inflammatory process, if we looked underneath the microscope, neutrophils and macrophages side by side. 00:48 The neutrophils are going away, the macrophages are coming on. 00:53 The neutrophils undergo apoptosis. 00:55 And the debris that they have generated up to that point also gets eaten by the macrophages. 01:02 So remember apoptosis creates little apoptonic bodies that have a little eat me signal on them, and the macrophages will gobble that up. 01:10 So they're going to be the definitive cleanup crew. 01:13 The neutrophils have come through and they've created a bigger mess. 01:16 They've cleaned up some of it. 01:18 But then macrophages which are longer lived, are going to be able to definitively clear the field. 01:26 There have also been extravasation of fluid and proteins, that's that increased vascular permeability, much of that will be taken up by the macrophages as well. 01:36 But we also have lymphatics that are in the tissues and fluids and proteins from the extravasated blood fluid will be taken up in the lymphatics and so we will eventually restore the normal amount of fluid in the extravascular space. 01:54 Macrophages at that point, hopefully everything's cleared up. 01:56 We're no longer infected, and the macrophages either to them become quiescent. 02:01 So they'll stay around. 02:03 Every time we've had an extravasation a macrophage, we leave a little bit behind as kind of sentinels for the next possible trauma. 02:12 If they don't stay around, they do have the capacity to wander into the lymphatics or even back into the blood vessels, and then leave the same. 02:22 The ones that stick around are going to be important for elaborating a variety of growth factors that are going to regulate fibroblast production of extracellular matrix, going to regenerate new blood vessels, and hopefully affect a complete repair. 02:38 So on this one slide, we're kind of looking at the total process of going from acute to chronic inflammation, and the emphasis here is on the macrophage. 02:49 It is the key cell for driving, repair, and for scarring. 02:54 So we'll talk about a lot of other cells, but the macrophage is the key player, the conductor, the field marshal for the healing response, the regenerative response, or the scarring response. 03:06 That's going to be happening in the tissue after injury.
About the Lecture
The lecture Going from Acute to Chronic Inflammation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Which of the following plays a key role in coordinating tissue repair and scarring?
- Macrophages
- Lymphocytes
- Neutrophils
- Mast cells
- Endothelial cells
What is the fate of neutrophils after the resolution of acute inflammation?
- They undergo apoptosis.
- They return to circulation through blood vessels.
- They return to circulation through lymphatics.
- They become quiescent and stay in the interstitial space.
- They differentiate into scavenger cells.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |