Playlist
Show Playlist
Hide Playlist
Glioma: Treatment
-
Strowd CNS Tumors Glioma.pdf
-
Download Lecture Overview
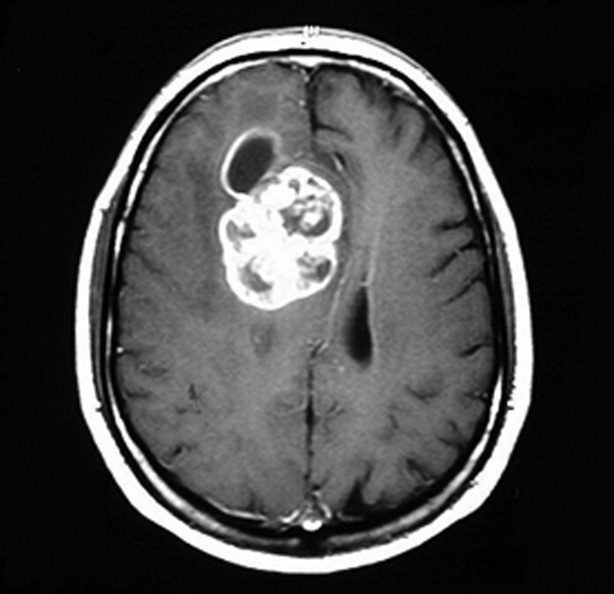
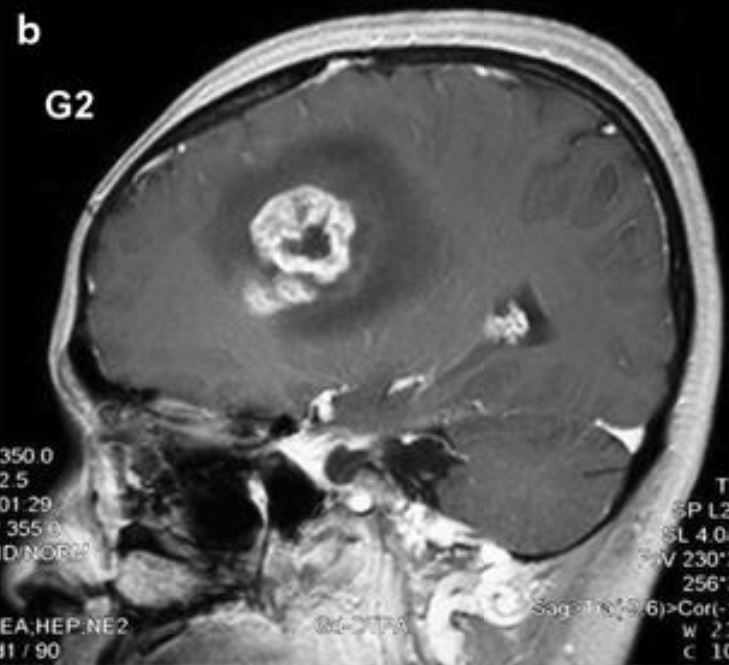
00:01 So we've made a diagnosis. 00:02 The patient presented, we did some imaging, we worked with the histology and genetic findings to establish a diagnosis. 00:09 How do we treat these gliomas? And how do we treat the most aggressive grade IV glioblastoma? Well, first patients have to recover after surgery. 00:18 And typically patients are given about four to six weeks for the incision to heal, and to recover function. 00:24 We want patients to be as strong before treatment as they can be, so that they can get through treatment as functional as possible. 00:32 After that four to six week recovery, most treatment regimens include some type of radiation, and we'll talk about radiation. 00:39 This is followed by a few week or four week recovery, and then that's followed by chemotherapy. 00:44 There are three types of chemotherapy. 00:46 Neoadjuvant chemotherapy is given prior to definitive treatment, which we don't tend to see or use with gliomas. 00:54 Concurrent chemotherapy is given at the same time as definitive treatment along with radiation. 00:59 And then adjuvant chemotherapy is given after definitive treatment. 01:03 And here we see typically for gliomas that's given after radiation therapy. 01:07 So this is how we're going to treat patients. 01:10 Let's dive into each one of these modalities and understand more, how we use those and what patients experience? First, let's think about, how patients do? A long time ago, the only treatment we had for gliomas was surgery. 01:24 And with no treatment or surgery alone, outcomes are extremely poor from high grade gliomas, typically grade IV gliomas with a median survival of only around four months. 01:35 These are the most aggressive of the brain tumors we will cover and can be very unresponsive to treatment, and even difficult without treatment. 01:44 Over time, radiation was added to our toolbox of treatments, and we saw an improvement in survival to nine months. 01:51 We got smarter about how much radiation to give? And currently give about 60 gray. That's how we dose radiation. 01:57 And that's a treatment dose of radiation for a brain tumor, with a median survival of around 12 months. 02:04 Over time, in decades ago, our field added certain types of chemotherapy, or wafers into the tumor, and some minimal gains in median survival until the addition of a chemotherapy that we'll talk a little more about in a minute called temozolomide, with a median survival of around 15 months. 02:21 The more coordinated our care is the better patients do. 02:24 And ultimately, the last treatment to be added to the regimen for patients with gliomas is called Tumor Treatment Fields. 02:30 And currently, the median survival for glioblastoma is around 20 to 24 months for around two years from diagnosis. 02:37 These are tough tumors that require a comprehensive and multidisciplinary group and need to be treated at an experienced center. 02:46 So how do we think about each of these treatments? Well, let's start first with surgery. 02:50 And I like to think about surgery in two ways. 02:53 They're surgery that take out golf balls, and they're surgery that scoop up sand. 02:58 And that's really the two types of tumors that we see on the brain. 03:01 Our grade I tumors are like those golf balls. 03:04 They're well circumscribed tumors that do not infiltrate the brain, they displace the brain, and can be plucked out with surgery. 03:12 Those are tumors that with a maximal surgery, or gross total resection, can be surgically cured without any adjuvant therapy, any additional treatment needed after surgery. 03:23 And that's the example of our grade I gliomas. 03:26 Grade II, III, and IV gliomas are infiltrating tumors. 03:30 They're much more like this sand dropped on a patch of grass. 03:34 You can see where most of the sand is and the surgeon can take that out with surgery, but there are granules of sand that you cannot see on the MRI, that the surgeon cannot take out with surgery, and they will need additional treatment after surgery. 03:48 So surgery is critical, as the backbone of diagnosis and management, but it's ineffective and eradicating, particularly the infiltrating lesions. 03:57 What's the goal of surgery? Well, we really have two goals. 04:01 One is to acquire tissue and make a diagnosis. 04:04 And the other is to remove tumor, and to cytoreduce or decrease the amount of tumor volume that is needed for subsequent treatment. 04:12 Acquiring tissue allows for diagnosis. 04:14 It allows for additional prognostication through the genetic testing, and may provide information on selecting specific therapies to target certain genetic events in tumors. 04:24 Cytoreduction is critical for removing tumor and decreasing the total amount of volume that will need to be treated after surgery. 04:33 What about radiation and chemotherapy? What's the role for those treatments after surgery? Radiation therapy works for the vast majority of tumors. 04:41 This is the backbone of therapy for gliomas. 04:45 And I like to think of radiation like Pringles, once you pop, you can't stop. 04:50 Everybody loves to Pringle, and all of these tumors need radiation therapy. 04:54 It is the backbone of treatment, that the vast majority of tumors will respond well too. 05:00 Chemotherapy is a little bit different. 05:02 Only a minority of tumors will respond to most chemotherapy, but those that respond will have an exquisite response. 05:10 I like to think of chemotherapy, like hot sauce. 05:13 Not everybody likes it, but those that like it just dump it on. 05:17 And the same is true for chemo. 05:19 We treat many tumors with chemotherapy, knowing that a minority will respond and those that do, often will have a dramatic response. 05:28 So let's think about how we stage in radiation and chemotherapy for the treatment of gliomas. 05:33 And we'll start with radiation. 05:35 We've talked in another lecture about the types of radiation therapy. 05:38 We talked about stereotactic radiosurgery, partial brain radiation, and whole brain radiation. 05:45 And typically the radiation that's given for a glioma is that middle, the partial brain radiation. 05:50 where we want a high dose delivered to the tumor, and also good treatment dose delivered to the margin where there may be tumor that we cannot see underneath the surface. 06:00 There are many types of chemotherapy regimens, and there's only two that I want you to know of. 06:05 One type of chemotherapy is temozolomide. 06:07 And we'll talk more about that in the next slide. 06:09 The other is a combination regimen called PCV. 06:13 And we combine these chemotherapies to radiation to help them work better. 06:18 For oligodendrogliomas, one of the regimens that you may see is the combination of radiation, followed after the end of radiation by this combination regimen, PCV, which we'll talk about in a minute. 06:29 For astrocytomas, typically, we would start again with radiation and after the completion of radiation, treat patients with temozolomide based chemotherapy. 06:38 And for glioblastoma, we put those things together. 06:41 So patients receive radiation with concurrent temozolomide, that means chemotherapy at the same time as the radiation, and then after that's completed chemotherapy alone. 06:51 You don't need to know each of the individual regimens, but want to get some understanding as to how these treatments are combined for certain diagnoses, and certain patients. 07:01 So let's learn a little bit about two of the most common chemotherapy regimens for gliomas. 07:06 The first is temozolomide. It's abbreviated, commonly TMZ. 07:11 It's an oral agent, it's a pill, and it's an alkylating agent. 07:15 It goes and intercalates DNA. 07:18 Side effects to consider, and side effects are important testable questions for board exams are nausea and myelosuppression. 07:25 And those are the things that we think about with many alkylating therapies. 07:30 In addition, alkylating agents have a potential risk long term of causing cancer, and typically, that would be leukemia. 07:37 And those are the three side effects that I'd be thinking about in a patient or a test question pertaining to temozolomide. 07:44 How about PCV? What is that? It's a combination chemotherapy regimen that consists of three medicines: Procarbazine, CCNU, and Vincristine. 07:55 And the other name for CCNU is Lomustine. 07:58 There are three chemotherapies. 08:00 Two of them are oral pills: The procarbazine and CCNU. 08:04 And one of them is an infusion or an injection, vincristine. 08:08 We think about a number of side effects. 08:10 Nausea and myelosuppression is seen with the two pills, procarbazine and CCNU, because those are alkylating agents and that's the same thing we saw with temozolomide. 08:19 Neuropathy is seen with vincristine and is very important to monitor because once the neuropathy develops, it cannot be reversed. 08:27 And then two interesting side effects are pulmonary fibrosis, which we can see with CCNU, and is a buzzword that can show up with that CCNU chemotherapy and also the risk of secondary malignancy. 08:39 So many chemo therapies are used throughout cancer. 08:41 These are two that are important to understand as we think about gliomas.
About the Lecture
The lecture Glioma: Treatment by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Which of the following is a potential side effect of temozolomide used to treat gliomas?
- Secondary malignancy
- Ototoxicity
- Pulmonary fibrosis
- Peripheral neuropathy
- GI upset
Which of the following is a potential side effect of PCV (procarbazine, CCNU, and vincristine) used to treat gliomas?
- Myelosuppression
- Hair loss
- Cardiotoxicity
- Flu-like symptoms
- Megaloblastic anemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |