Playlist
Show Playlist
Hide Playlist
Glioma: Grading with Tissue Sample
-
Strowd CNS Tumors Glioma.pdf
-
Download Lecture Overview
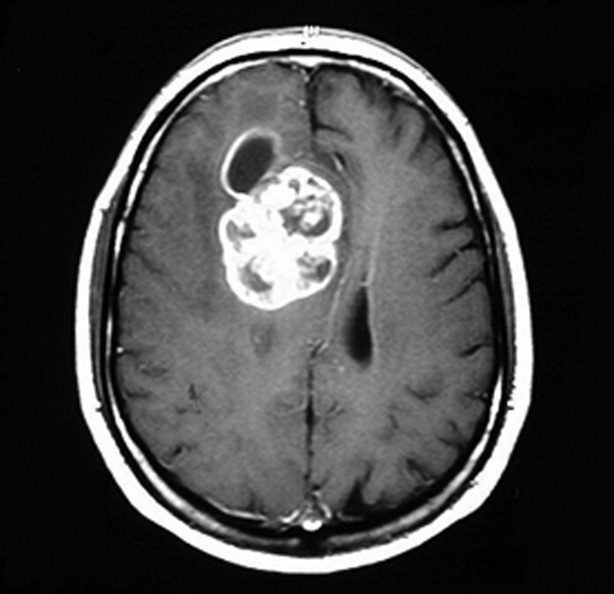
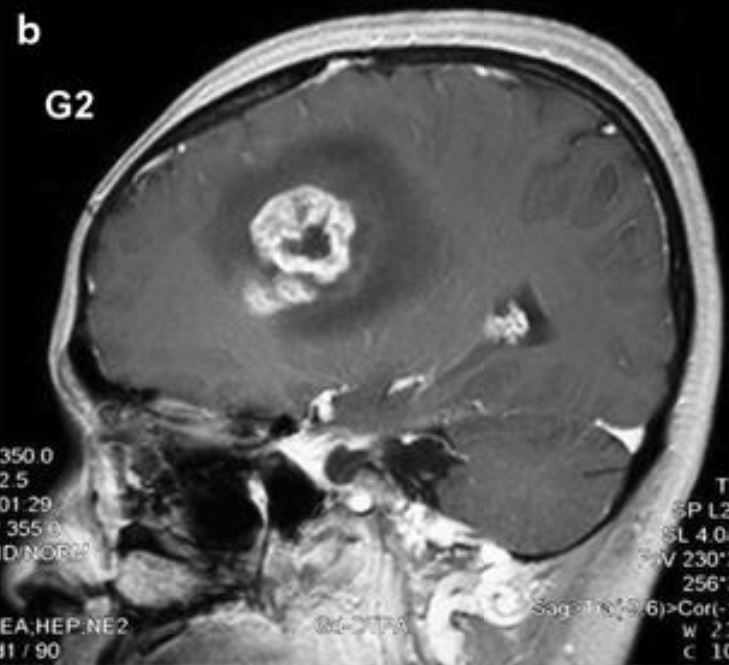
00:01 So after the imaging evaluation, we need to figure out, what is this tumor? And definitively diagnose it with tissue, and begin the treatment process. 00:09 And the mainstay of those two goals is really surgery. 00:13 So let's talk more about the types of surgery that we use, and why we use those for gliomas? Well, the goals of surgery are number one to establish a diagnosis. 00:23 Imaging may give us a concern about what this is, and we may be pretty sure, but ultimately, a definitive tissue diagnosis is required to treat and manage that patient with a suspected glioma. 00:35 The second thing is we'd like to help the patient. 00:38 And many of these tumors are large, and pressing on surrounding structures of the brain causing symptoms or seizures. 00:43 And so a second goal of surgery is to relieve symptoms of mass effect, edema, and improve patient symptoms. 00:51 For most cancers, and a glioma is a type of cancer, we think about staging. 00:56 And staging makes sense. 00:58 You may have learned of the TNM scale. 01:01 The tumor size, the number of nodes, and the degree of metastatic disease, and that helps us evaluate, to diagnose, and then to manage patients who may have a cancer. 01:12 This doesn't work so well for gliomas, because size doesn't matter. 01:16 Location matters. 01:18 And really small tumors in the brainstem are small in size, but bad in symptoms. 01:23 The brain does drain, but there is not an avid lymph node or lymph node drainage in the brain that we can follow that will guide us into the degree of invasion of those tumors. 01:33 And brain tumors, gliomas, don't metastasize. 01:36 So that TNM scale really doesn't help us. 01:39 Instead, when we're evaluating gliomas, we grade those tumors. 01:43 And that requires a pathologist to definitively and comprehensively evaluate that tumor under the microscope. 01:50 Pathologic grading is based on the cell morphology. 01:53 The appearance of the tumor cells, on the slide, and the degree of aggression or invasion that is seen in that sample. 02:02 Let's look at some examples of the histologic slides for patients with gliomas. 02:07 Here we see an example of an astrocytoma. 02:10 This tumor is a tumor that may arise from the astrocytes the most abundant cells in the brain. 02:16 And those astrocytes are typically intermixed around normal neurons, and in low-grade astrocytomas, this appears to look very similar to normal brain. 02:25 In higher-grade astrocytomas, we see many cells packed in together. 02:30 Oligodendrogliomas have a very classic histologic appearance that you should know about. 02:36 This is the fried egg appearance. 02:38 As a result of fixation, when these oligodendrocytes are fixed, there is a halo that occurs around the nucleus. 02:46 So we see a small blue nucleus and a clear halo that looks like a fried egg. 02:52 And so oligodendrogliomas histologically have a fried egg appearance. 02:57 Ependymomas are often packed cellular tumors with rosettes. 03:02 So how do we grade those tumors? When the pathologist is evaluating the tumor histologically, how do they assess its grade or its aggressiveness? Well, grade I tumors are not infiltrating. 03:14 They are tumors that sit inside the brain and displace the normal brain. 03:18 They're well circumscribed. 03:20 And we can see that both on imaging and histology. 03:23 And there are two important histologic buzzwords that I'll have you know about. 03:27 You don't need to know what causes these but you do want to associate them with grade I gliomas in your mind. 03:33 And that's Rosenthal fibers and these things called eosinophilic granular bodies. 03:38 There are specific histologic findings that suggest a diagnosis of a grade I glioma. 03:44 What are the types of grade I gliomas? Well, one is a pilocytic astrocytoma. 03:49 And you're going to associate that in your mind. 03:51 Pilocytic astrocytomas are grade I gliomas, and grade I gliomas the most common is a pilocytic astrocytoma. 03:58 That's an important example of a grade I glioma to know. 04:02 There are other types. 04:03 The subependymal giant cell astrocytoma, this dysembryoplastic neuroepithelial tumor or a DNET, and a ganglioglioma. 04:12 But the one I want you to remember that grade I glioma is a pilocytic astrocytoma. 04:19 The grade I tumors are very different from grade II, III, and IV gliomas. These are infiltrating tumors. 04:24 They start in a focus and grow into an evade into the brain. 04:28 So they're called infiltrating. 04:30 We typically see hypercellular tumors and nuclear atypia. 04:34 The nuclei don't look right in these neoplastic cells. 04:39 Some examples of grade II gliomas are the diffuse infiltrating glioma, a pleomorphic xanthoastrocytoma, which is really rare and I don't need you to remember that but just know of it. 04:50 And something called the pilomyxoid astrocytomas. 04:53 But a diffuse infiltrating low-grade glioma is going to be our prototypical grade II glioma that I'd like you to know. 05:00 What about grade III tumors? These are also infiltrating gliomas that are hypercellular. 05:06 There's too many cells growing into the brain. 05:09 These tumors are actively growing and we can see that histologically. 05:13 There's increased mitotic activity. We see actively dividing cells. 05:17 And when that is seen that indicates that this tumor is a grade III and is more aggressive. 05:22 There can be elevated molecular markers of proliferation, Ki-67 and MIB-1 are proteins that are expressed in cells that are dividing, and so increase Ki-67, and MIB-1 tells us that this tumor is growing, and this is a grade III glioma. 05:39 The example I want you to remember of a grade III glioma is called the anaplastic astrocytoma, or the anaplastic oligodendroglioma. 05:47 Those are grade III astrocytomas, or oligodendrogliomas. 05:51 And we know that because of that active proliferation that the pathologist sees under the microscope. 05:56 And the last and maybe the most important glioma to know is the grade IV glioma, which we called glioblastoma. 06:04 Again, this is an infiltrating tumor that grows into the brain. 06:07 There are too many cells that do not look correct. 06:09 There's hypercellularity, and nuclear atypia. 06:12 The cells are actively dividing. We see mitosis. 06:15 And there are two histologic features that are pathognomonic for glioblastoma. 06:20 Meaning that if you hear of these, that means it's a glioblastoma. 06:23 And you should know these. 06:24 The first is vascular proliferation. 06:27 There is excess blood vessels in these tumors. 06:29 And that's what causes them to enhance avidly with contrast, and then something called pseudopalisading necrosis. 06:36 And what's going on to cause that finding is the tumor cells are rapidly dividing, faster than blood can be supplied. 06:44 And so there's areas of cell death or necrosis, and around the necrosis, around the cell death are actively growing and dividing tumor cells growing away from those central hypoxic areas where the tumor cells can't grow. 06:56 And that's very specific for this diagnosis of glioblastoma. 07:00 So that's how we think of, and look at, and diagnose these tumors, histologically.
About the Lecture
The lecture Glioma: Grading with Tissue Sample by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
What is the most important thing to consider when staging gliomas?
- Location
- Tumor size
- Number of nodes
- Depth of invasion
- Metastasis
Which of the following brain tumor types is composed of a cell type with a small blue nucleus surrounded by a clear halo described as having a "fried egg" appearance?
- Oligodendroglioma
- Astrocytoma
- Optic glioma
- Meningioma
- Ependymoma
Which of the following brain tumor types is composed of cells arranged in rosettes?
- Ependymoma
- Astrocytoma
- Oligodendroglioma
- Schwannoma
- Glioblastoma
Which of the following histologic findings suggests a grade IV glioma (GBM)?
- Pseudopalisading necrosis
- Nuclear atypia
- Eosinophilic granular bodies
- Well-circumscribed mass
- Elevated Ki-67/MIB-1
Which of the following histologic findings suggests a grade I glioma such as pilocytic astrocytoma?
- Rosenthal fibers
- Increased vascular proliferation
- Mitotic figures
- Infiltrating glioma
- Hypercellularity
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |