Playlist
Show Playlist
Hide Playlist
GERD: Management and Surgery
-
Slides GERD General Surgery.pdf
-
Download Lecture Overview
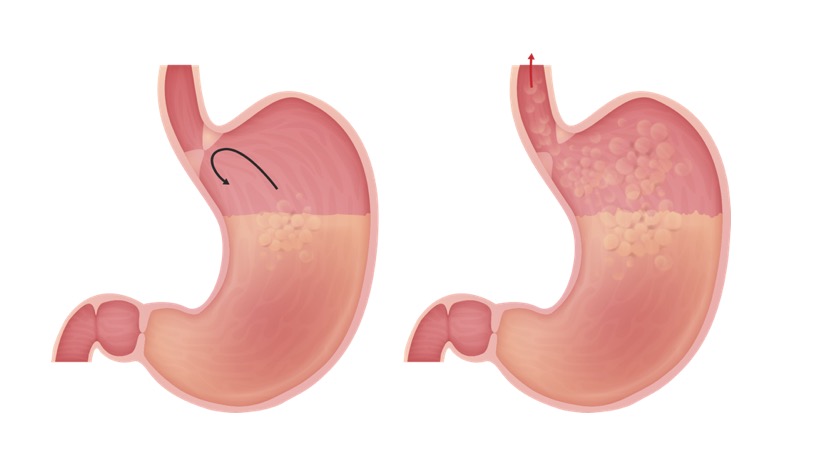
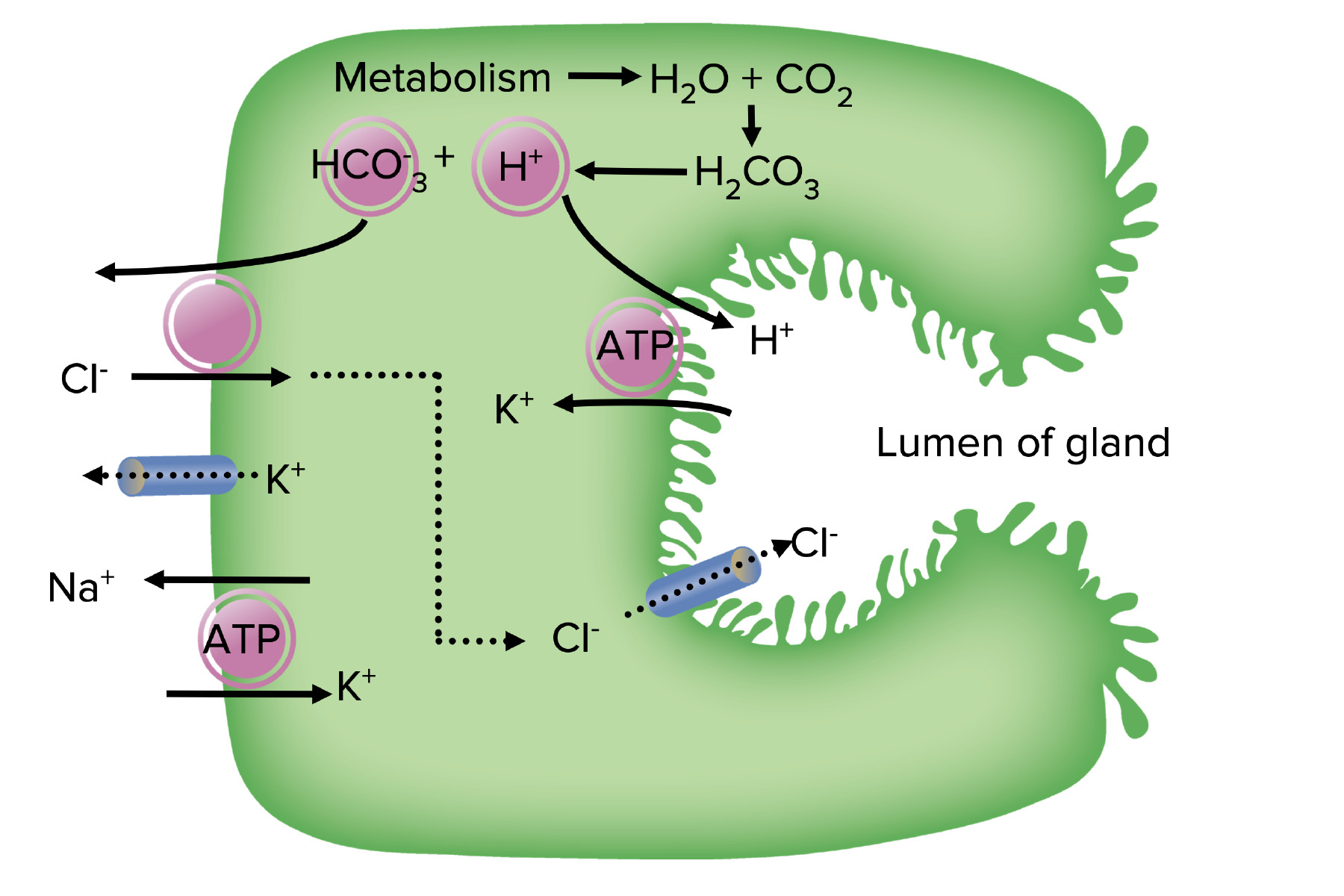
00:01 What are some of the initial management? Well, we want to do anything we can to reduce the acid. 00:07 Acid reduction maneuvers include proton pump inhibitors, histamine 2 receptor antagonist. 00:14 Recall that proton pump inhibitors and histamine 2 receptor antagonist work in two different mechanisms but the common pathway is to decrease hydrochloric acid secretion. What are some other methods of acid reduction on reflux: weight loss, elevation of the head during sleep, and avoiding smoking and alcohol. Weight loss and smoking and alcohol are tied to a decrease in your lower esophageal sphincter tone. 00:46 The lower esophageal sphincter, although not technically a sphincter itself does gate control of the amount of reflux into the esophagus. What’s the association of H. pylori with reflux disease? Here’s the sequence and a schematic of how I think about H. pylori. If H. pylori is classically associated with peptic ulcer disease and that there is a link between H. pylori and GERD then there is some suggestion that H. pylori is detected along with GERD, better symptomatic relief if the H. pylori is treated. What does that mean? There’s an association between H. pylori and gastritis and GERD. Therefore, oftentimes by treating the H. pylori, patients with GERD also have a resolution or at least an improvement in their symptoms. Barrett's esophagus, pay particular attention. Barrett's esophagus is a complication of chronic reflux disease. 01:44 It is defined by metaplastic columnar epithelium replacement of the normal squamous epithelium. 01:53 Most importantly, Barrett's esophagus predisposes to esophageal cancer. 02:04 Most importantly, Barrett's esophagus predisposes to esophageal adenocarcinoma. 02:06 When is surgery offered? Surgery is offered for complications of reflux disease. Again, like many of the diseases we have discussed in these lecture modules of surgery, non-surgical management or medical management is usually the first line. When the patients have failed medical management and require surgery for GERD, it’s usually because of a complication. Here are some complications and indications for surgery: failed medical management, Barrett's metaplasia or Barrett's esophagus, and importantly, severe esophagitis. 02:47 Severe esophagitis can lead to strictures and dysphagia. When you deem the patient necessary of surgery, a classic description of a Nissen fundoplication is something that we would offer the patient. 02:59 This is usually performed laparoscopically as a 360 degree wrap around the GE junction. 03:06 This is performed by mobilizing the greater curvature of the stomach. It has been demonstrated to offer the greatest long term durability in terms of symptomatic relief. Note that there are several goals of a Nissen fundoplication. Number 1, it keeps the GE junction in its anatomic space. Number 2, it also maintains the lower esophageal sphincter tone preventing chronic reflux. Here are some important clinical pearls. Patient may experience dysphagia if the fundoplication is too tight. 03:40 How do you know if the fundoplication is too tight? Well, immediately after surgery, the patient may have difficulty belching or tolerating their own saliva. This may also be coupled with abdominal pain. 03:54 Further down the line, the patient may experience dysphagia. Once the fundoplication scarring has formed, this can be diagnosed using endoscopy. For your examination, recognize that Barrett's esophagus predisposes to esophageal cancer due to chronic exposure to gastric acid. Thank you very much for joining me on this discussion of gastroesophageal reflux disease.
About the Lecture
The lecture GERD: Management and Surgery by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which one of the following is NOT commonly recommended to reduce the symptoms of gastroesophageal reflux disease?
- Docusate sodium
- Proton pump inhibitor
- Avoid smoking
- Avoid alcohol
- Weight loss
What are the mechanisms of action of proton pump inhibitors and histamine-2 receptor antagonists?
- Both decrease secretion of hydrochloric acid
- Both decrease the pH of hydrochloric acid
- Both are basic substances which act to neutralize the overall pH in the stomach
- Both increase the tone of the lower esophageal sphincter
- Both increase stomach motility
Which of the following correctly defines Barrett’s esophagus?
- Metaplastic columnar epithelium replacement of squamous epithelium in the esophagus due to chronic gastric reflux
- Metaplastic squamous epithelium replacement of columnar epithelium in the esophagus
- Metaplastic esophageal epithelium replacement of columnar epithelium in the stomach
- Metaplastic squamous epithelium hyperplasia in the esophagus
- Metaplastic columnar epithelium hyperplasia in the stomach
Which of the following is an indication for surgery for complicated gastroesophageal reflux disease?
- Severe disease refractory to medical management
- Helicobacter pylori infection
- Water brash
- Chest pain accompanying initial reflux symptoms
- Esophageal pH of less than 4 at any point during 24-hour monitoring
Immediately after surgery for severe esophagitis, a patient reports difficulty belching, increased saliva, and abdominal pain. What is the likely cause of these symptoms?
- The Nissen fundoplication procedure has wrapped the fundus of the stomach too tightly around the gastroesophageal junction.
- These are normal anticipated symptoms after Nissen fundoplication, and the patient should be reassured.
- Failure of the Nissen fundoplication and worsening of reflux symptoms
- Dehiscence of the surgical anastomosis
- The laparoscopic band is placed too high around the stomach fundus.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |