Playlist
Show Playlist
Hide Playlist
Functional Thyroid Disorders in Pregnancy
-
Slides Thyroid and Reproduction.pdf
-
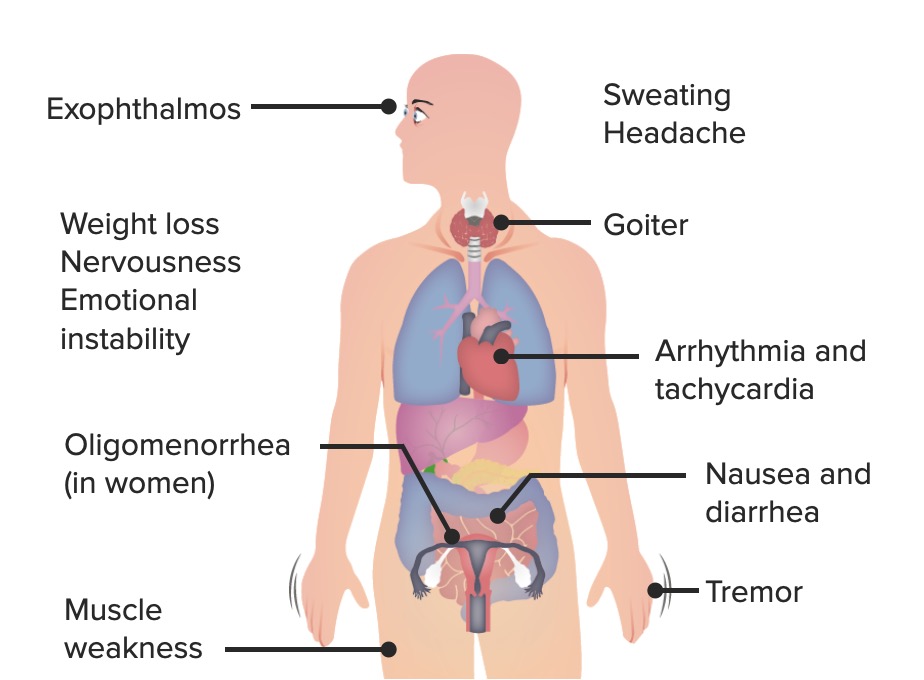
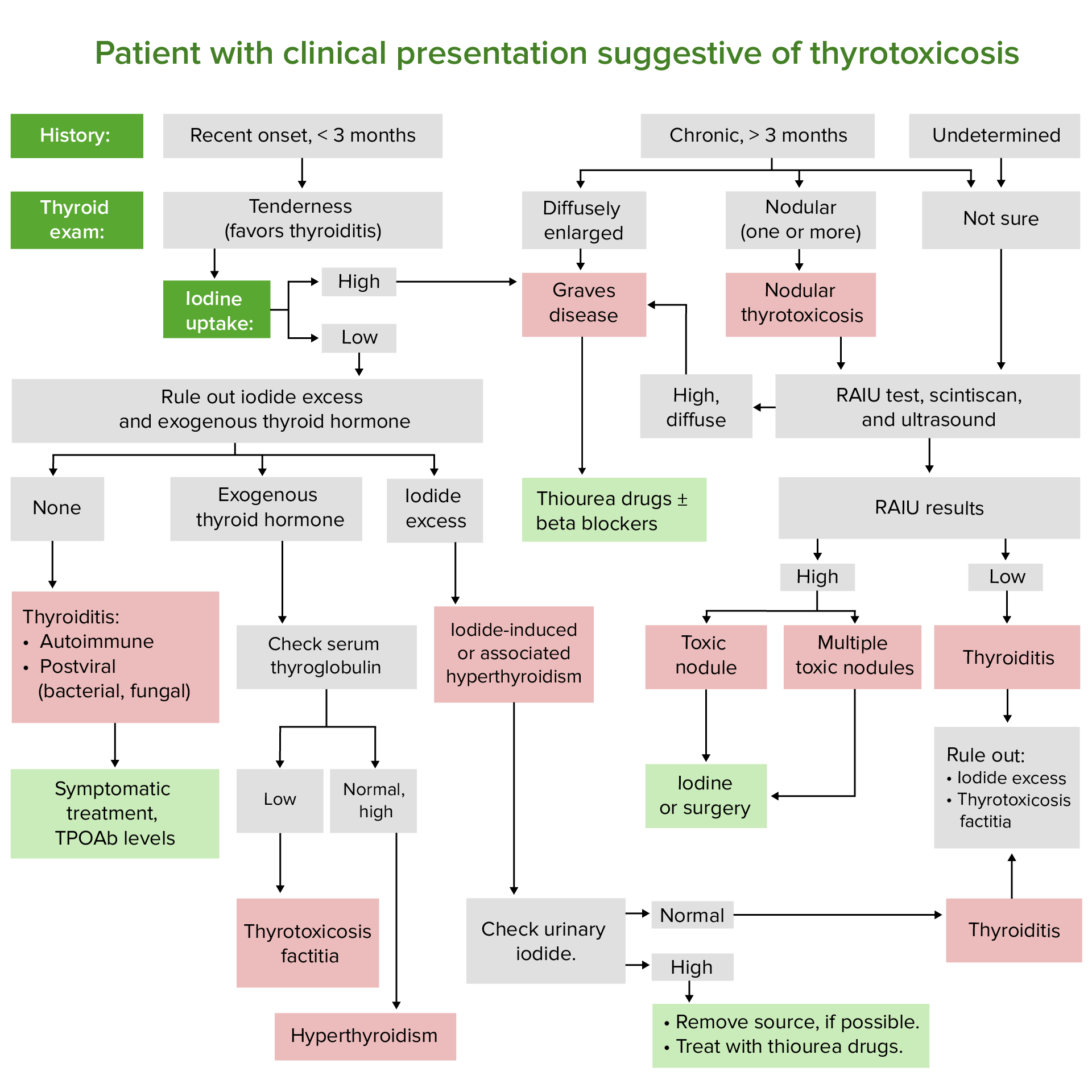
Download Lecture Overview
00:00 Let's now review maternal thyroid function in pregnancy. In pregnancy, we have increased renal clearance of iodine and this is increased because of the increased GFR. GFR stands for glomerular filtration rate. There are also substantial amounts of iodine and iodothyronine that are transferred to the fetus that's developing. Thyroid-binding globulin, TBG, increases because of the high levels of estrogen during pregnancy and there are mean concentrations of T4 and T3 increased 10 to 30%. 00:36 HCG production from the syncytiotrophoblast is very similar to TSH and this can cause some thyroid suppression. Remember, if you are hypothyroid during pregnancy, then you need to increase the dose of levothyroxine by 30% to the increased demands of pregnancy. This is increasing by 20 to 50 mcg daily in a pregnant patient as soon as her beta-hCG is positive. Let's now review the functional thyroid disorders in pregnancy. Let's first review thyrotoxicosis. This is a clinical and biochemical state that can result from an excess production of thyroid hormone from any cause. 01:18 Hyperthyroidism can actually cause thyrotoxicosis because the thyroid gland is hyperfunctioning and thyroid storm is one of the very few medical emergencies that we have in endocrine and it's characterized by a severe acute exacerbation of the signs and symptoms of hyperthyroidism. I've actually had a patient with thyroid storm and she had gestational trophoblastic disease that actually precipitated her thyroid storm. Let's review now hyperthyroidism in pregnancy. It occurs in 0.05% to 2% of all pregnancies. Grave's disease is the most common and accounts for 95% of all cases. Remember that the disease is mediated by IgG antibodies that can cross the placenta and post a risk for the fetus and can cause autoimmune-mediated thyroid dysfunction and if you are an endocrinologist you need to alert the OB/GYN to this and if you are an OB/GYN you need to alert the pediatricians to this. Let's now review how hyperthyroidism, so too much coffee, remember, can actually affect the female reproductive system and pregnancy. So hyperthyroidism has been linked to infertility. It's also been linked to adverse prenatal outcomes. The adverse prenatal outcomes are preeclampsia, cardiac failure, thyroid storm which we just discussed, and spontaneous loss. There are fetal effects as well as we discussed previously. You can have preterm delivery, low birth weight, intrauterine growth restriction, and increased perinatal mortality. Let's review thyrotoxicosis in pregnancy. Again, the major culprit is Grave's disease which is an autoimmune disorder. You can also have thyroiditis, toxic multinodular goiter, solitary toxic nodules, gestational trophoblastic neoplasia, struma ovarii which is tissue that is thyroid tissue elsewhere than where it should be and oddly enough it's found sometimes in the ovary. 03:27 Exogenous thyroid hormone so the patient's taking thyroid hormone more than she should or she is surreptitiously taking it to maybe lose weight. So you might want to ask about that in the history. Iodine-induced thyrotoxicosis, TSH-secreting pituitary adenoma, gestational hyperthyroidism, hyperemesis gravidarum which is reviewed in other lecture, and familial gestational hyperthyroidism. 03:54 Let's review what the presentation looks like for Grave's disease. Remember they kind of have these popping eyes and they have lid lags, they can't quite close their eyelids, they may also have some dermopathy as well and usually the dermopathy is localized or pretibial edema. Let's now review hypothyroidism. So remember this patient is slow, their metabolism is slow because their thyroid is not functioning adequately. Again, these patients can have complications of pregnancy, 0.6% of all their pregnancies have some complication. This hypothyroidism is more common in women who have other autoimmune diseases such as type 1 diabetes and if a patient presents to the office wanting to get pregnant with type 1 diabetes, the first thing you need to do is check her TSH. Hashimoto's disease is a chronic autoimmune thyroiditis that leads to hypothyroidism, it's the most common in developed countries such as the US and worldwide iodine deficiency is the most common cause. So their diet is lacking iodine which leads to hypothyroidism because iodine is necessary to make thyroid hormone. These pregnancies that are associated with hypothyroidism are complicated by preeclampsia-associated issues as well as low birth weight, placental abruption, preterm birth, and stillbirth. Let's now review the causes of primary hypothyroidism. So the gland has an issue, not anything before the gland. This is usually due to an iodine deficiency, chronic autoimmune thyroiditis, silent postpartum thyroiditis, prior treatment for hyperthyroidism that actually destroys the thyroid and now they become hypothyroid. Prior high dose of external beam neck radiation so they've had some type of cancer that caused them to have radiation that destroys the thyroid. It can be infectious so you can get an infectious thyroiditis, subacute thyroiditis or you have some thyroiditis and then you go into a hypothyroid state, thyroid agenesis or dysgenesis so embryologically their thyroid is not developed. They can have drug-induced hypothyroidism, dietary goitrogens, or they can have organification of enzymatic defects. Let's now review the secondary causes of hypothyroidism in pregnancy. One, pituitary adenomas can occur and cause hypothyroidism but it's a secondary cause because it's not in the gland that's the problem, it's actually in the pituitary. You can have pituitary necrosis and hemorrhage, you can have lymphocytic hypophysitis, you can have central nervous system sarcoidosis, you can have a prior hypophysectomy, you can have a radiation that causes anterior pituitary issues, you can have supracellular or paracellular masses or trauma or injury to the pituitary or hypothalamus.
About the Lecture
The lecture Functional Thyroid Disorders in Pregnancy by Lynae Brayboy, MD is from the course Reproductive Endocrinology.
Included Quiz Questions
A 25-year-old woman comes with a history of a distended abdomen and 3 months of amenorrhea. She complains of tremors and heat intolerance. Abdominal ultrasound shows a pelvic mass. What is the probable cause of her symptoms?
- Struma ovarii
- Metastasis of thyroid cancer
- Graves disease
- Autoimmune thyroiditis
- Hyperthyroidism in pregnancy.
Which of the following is NOT a fetal effect of maternal hyperthyroidism?
- Cretinism
- Pre-term delivery
- Low birth weight
- Intrauterine growth retardation
- Increased perinatal mortality
Which of the following is the most common cause of primary maternal hypothyroidism in developed countries?
- Hashimoto's thyroiditis
- Iodine deficiency
- Postpartum thyroiditis
- Drug-induced hypothyroidism
- Thyroid agenesis
Which of the following is an example of primary hypothyroidism in pregnancy?
- Drug-induced hypothyroidism
- Pituitary adenoma
- Empty sella syndrome
- Lymphocytic hypophysitis
- CNS sarcoidosis
Which of the following is the most common cause of maternal hyperthyroidism during pregnancy?
- Graves' disease
- Toxic nodular goiter
- Struma ovarii
- Iodine-induced thyrotoxicosis
- Autoimmune thyroiditis
Customer reviews
2,5 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
no es muy util, solo enlista etiologias, seria mejor enfocar mas en fisiopatologia de las mas importantes
This lecture is not good at all. Please explain the mechanism of the symptom.