Playlist
Show Playlist
Hide Playlist
The Febrile Baby: Urinary Tract Infection (UTI), Bacteremia & Meningitis
-
Slides Febrile Infant .pdf
-
Download Lecture Overview
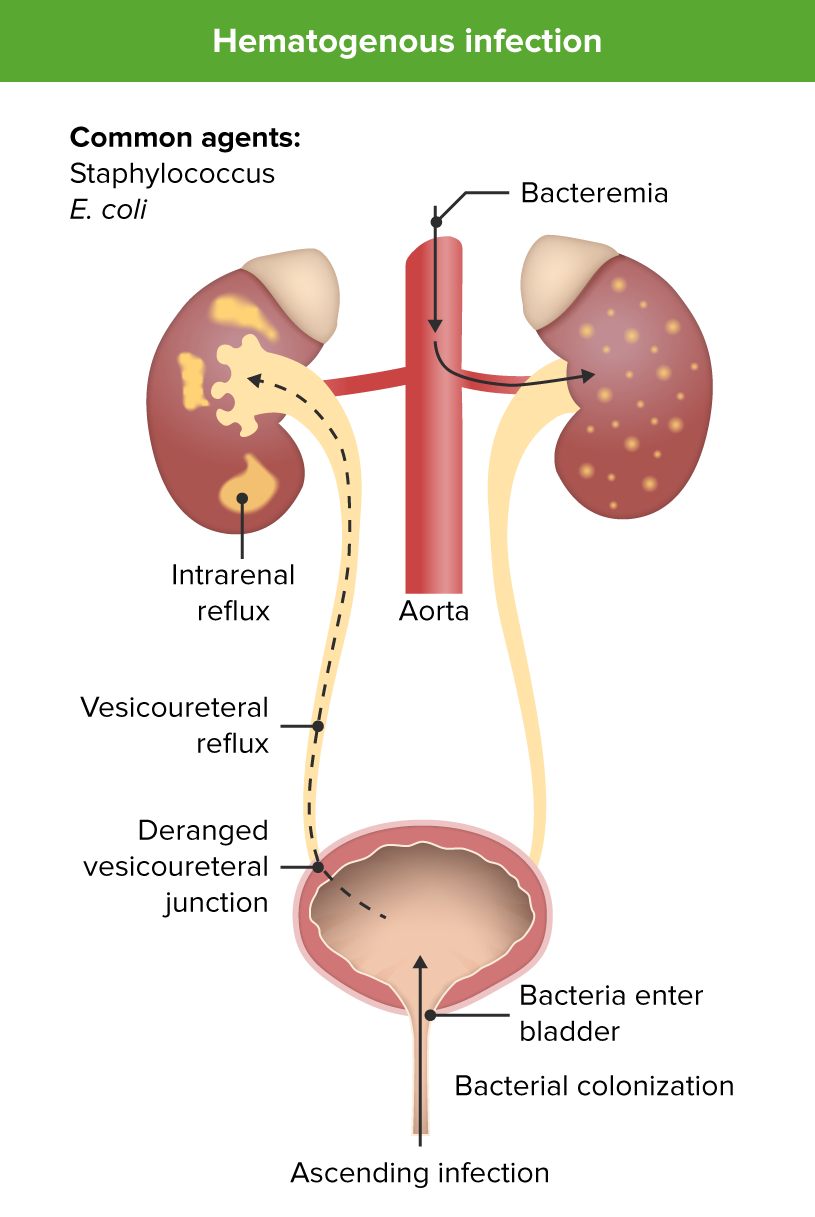
00:00 Okay, let's get away from HSV because I really want to focus on bacterial causes of children being sick in the hospital with a fever. The most common by far risk is urinary tract infection and this typically happens between 5 and 10% of the time, perhaps 10% in the first month and 5% after that. Bacteremia is relatively rare, about only 1% of the time, and meningitis is even rarer than that. So, the bacteria that cause these illnesses are very much the same, they're bacteria that the child is exposed to during the delivery process. Delivery is not a sterile phenomenon as you probably seen if you've been at one. So there are risks for mostly fecal organism such as E. coli or vaginal organisms such as group B strep especially in GBS positive mothers who are undertreated or untreated. Strep pneumoniae is not a typical bacteria that kids are _____ at the time of birth but it absolutely can cause sepsis in these children, although it's much less likely than in an older child. Likewise, Neisseria meningitidis is incredibly rare to get as a result of the birthing process but can rarely happen. Enterococcus is more of a fecal as is Klebsiella and we're seeing more and more Staph aureus in these newborns as we're seeing more aggressive Staph aureus types like MRSA or resistant Staph aureus, we are seeing it now and then and there can sometimes be outbreaks in newborn nurseries. Okay, I'm worried about urinary tract infection because that's the most common cause of bacterial illness in these children. What do I do? Whenever we get a test, we want to ask "Is it sensitive or specific?" In the case of this, we have 2 ways we can check labs in these kids. We can get a bag or we can get a catheter. If a child has a urinary tract infection, the bag is more sensitive. It's more likely to be positive. 02:07 If a child does not have a urinary tract infection, the cath is more likely to be negative. 02:13 It's more specific. In general, in the United States, we've decided that the cath specimen is superior. Now there are some ways you can work around this. If you have time you might bag the child and if the bag is negative then you're done and then proceed the catheterization if it's positive but most centers just go straight to catheterization or alternatively if you're incapable of getting urine any other way, you might do a suprapubic tap. That's where we insert a needle directly into the bladder through the abdominal wall to get the urine. It's actually a fairly safe procedure, although how successful it is depends on the experience of the practitioner but in general in the United States we prefer to go to cath or suprapubic tap as opposed to what they recommend in England. The reason we went that way is because there is more and more a feeling that these urinary tract infections are not as serious as we've previously suspected. 03:12 Kids tend to get better and many times it's not truly a UTI but it's bacteriuria, a benign shedding of bacteria in the urine. Okay, if we get that urine we're going to send it for a urinalysis and the urinalysis has several aspects on it that tell us whether the child is likely to have the disease. Remember, the more tests you get you improve your sensitivity and you lose your specificity. So if we look at the individual elements you can see that these all have different amounts of sensitivity and specificity. The one I would call your attention to is nitrites. It's 98% specific. That means if you have a positive nitrite on your urine dip, it's very likely that child has a UTI. Overall, the UA is a very sensitive test. It's 97% sensitive and has a high false positive rate, 30% false positive rate. So if a patient has UTI, it's almost always positive but it can be positive in normal individuals. Remember those 3 numbers. How do we approach bacteremia? Very ill children may have overwhelming bacteremia or bacterial sepsis and this is more common in infants than it is in older children. Untreated sepsis can lead to shock and death. So we do worry about bacteremia. What's the likelihood of bacteremia in a very well-appearing patient? It's very unlikely. True bacteremia is rare and when real may even resolve untreated. Remember, you are probably bacteremic transiently yesterday when you brushed your teeth. Okay, so we need test that can tell us quickly whether a child is at risk for bacteremia so we can distinguish well-appearing children who we should worry about versus those who we shouldn't and there are several tests out there. The procalcitonin is probably the best test, but it is expensive, and not available at all centers. The CRP is a good test for predicting bacteremia, but not perfect. The white blood cell count is not at all accurate, but is still eroneously used at many centers. 05:24 The white cell count is no better than a flip-of-a-coin at predicting whether a child has a bacterial infection or not. 05:31 Coming soon to a theater near you is blood PCR. 05:36 I suspect this may 1 day replace what we currently use as the goal standard test, which is culture.
About the Lecture
The lecture The Febrile Baby: Urinary Tract Infection (UTI), Bacteremia & Meningitis by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of UTI, Bacteremia and Meningitis
- Diagnosis of Urinary Tract Infections
- Diagnosis of Bacteremia
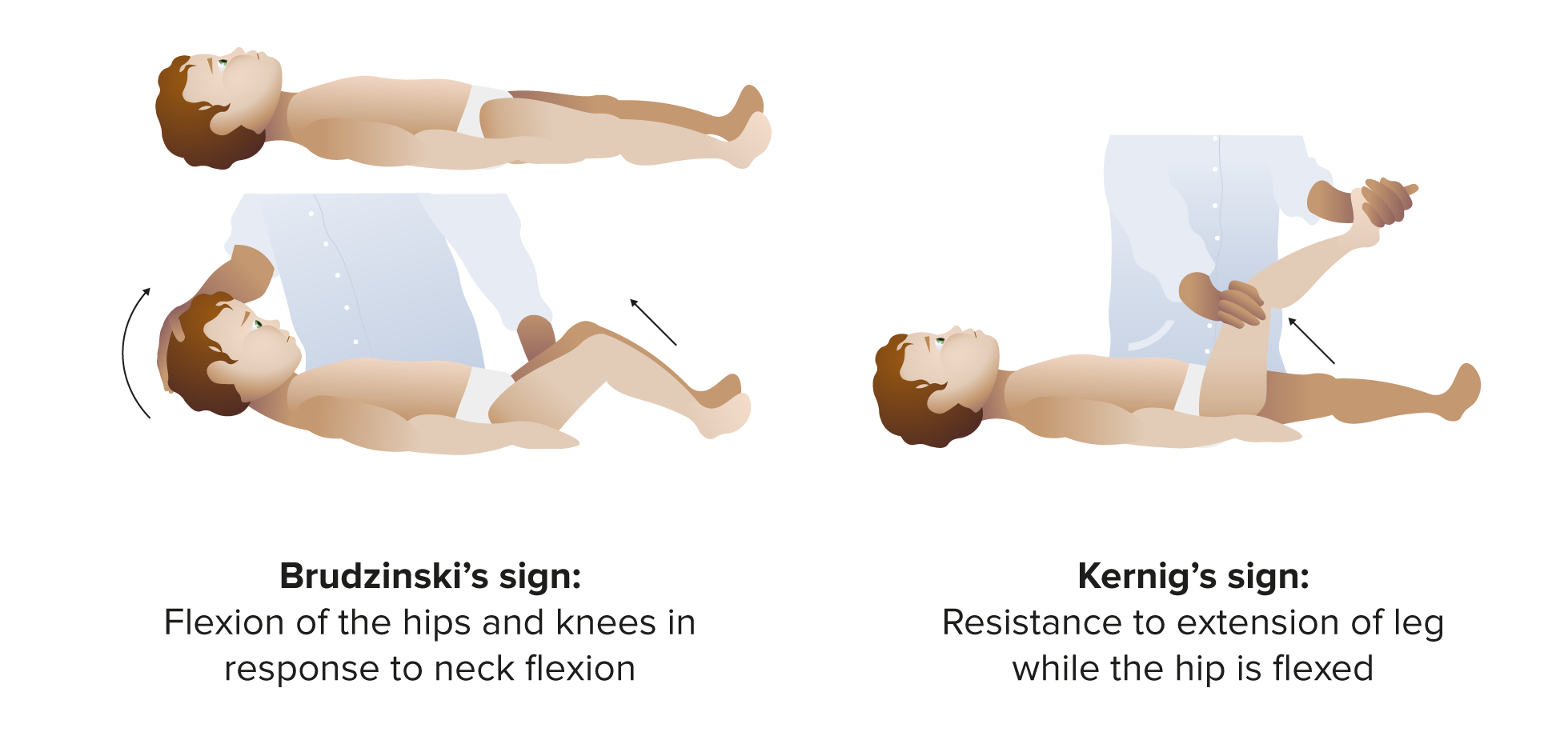
- Diagnosis of Meningitis
Included Quiz Questions
Which of the following is the most common cause of bacterial illness in young infants?
- Urinary tract infections
- Pneumonia
- Meningitis
- Bacteremia
- Cellulitis
How does Staphylococcus aureus infection most commonly present in the newborn?
- Osteomyelitis
- Meningitis
- Eye infections
- Rashes
- Runny nose
Which of the following is the gold standard for diagnosing meningitis?
- CSF bacterial Culture
- Cell count of CSF
- CSF glucose
- Gram stain of CSF
- CSF protein
Which of the following component of a urinalysis has the highest specificity for the diagnosis of a urinary tract infection?
- Nitrite test
- Elevated leukocyte count
- Presence of bacteria
- Positive leukocyte esterase test
- Overall interpretation of urinalysis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture! I learned tons. It shows that the instructor masters the topic and is able to give a clear and easy-to-understand picture. I now feel much more confident for these situations and more able to integrate the local guidelines now that I understand better the general concepts. Thanks!