Playlist
Show Playlist
Hide Playlist
Examination of the Abdomen
-
Reference List Physical Examination.pdf
-
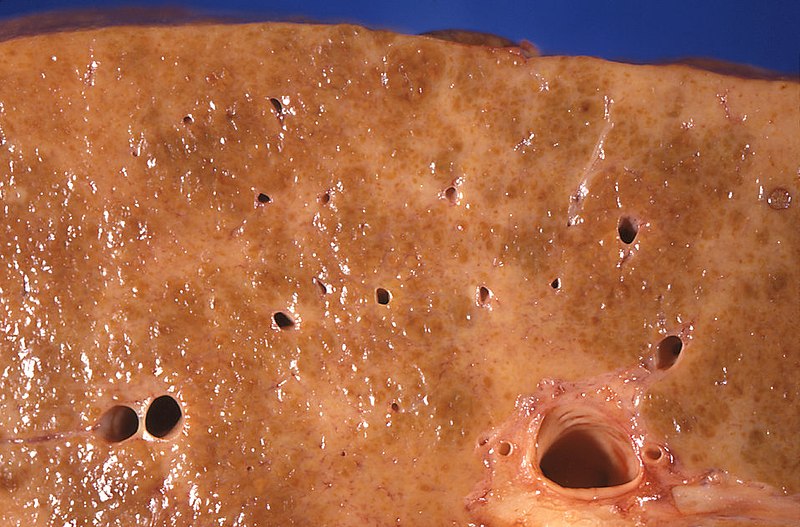
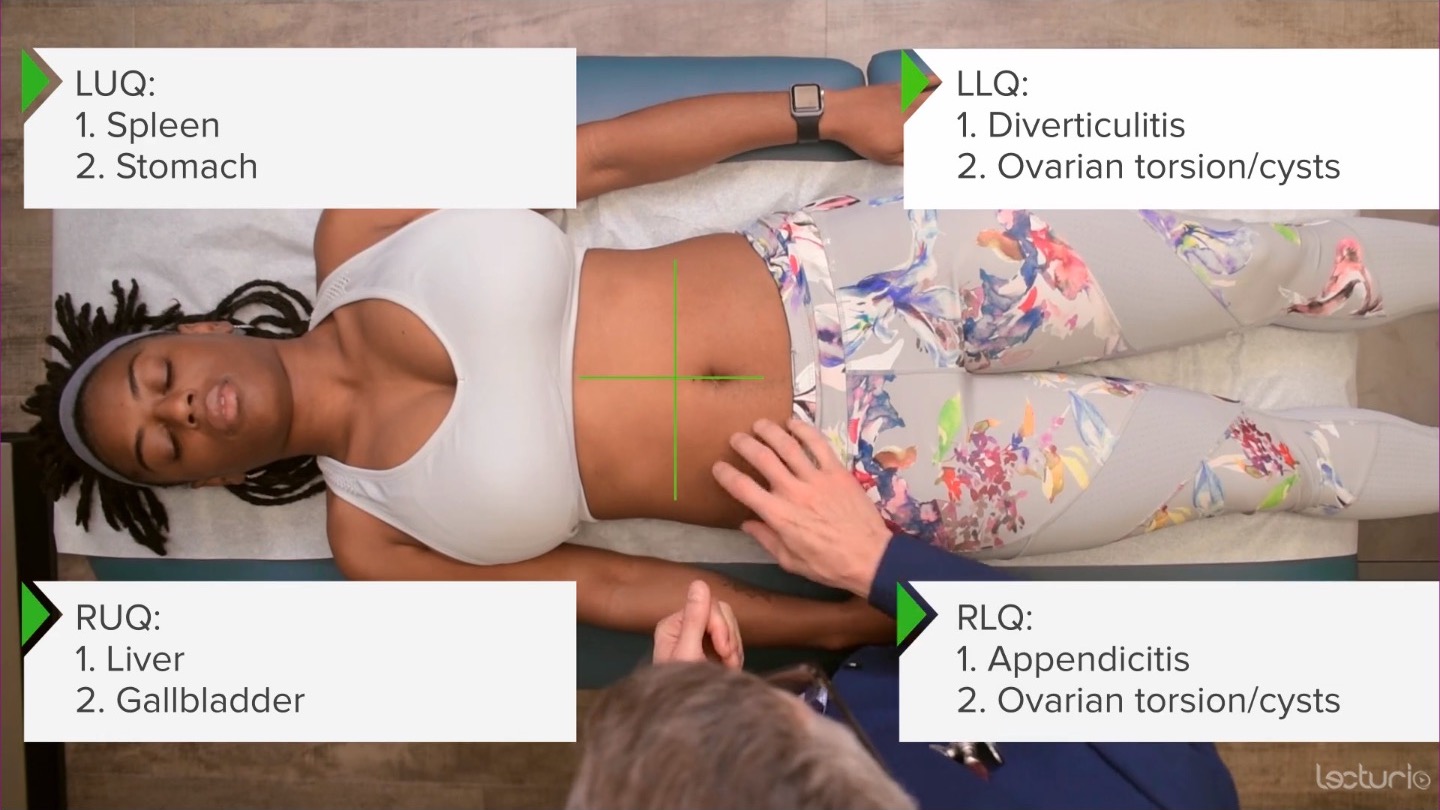
Download Lecture Overview
00:01 Alright, so next up, we're going to launch into the abdominal exam. 00:04 And like many systems that we're talking about in this course, it always starts with inspection. 00:08 So starting off from taking a look at her abdomen, the things that I really want to attend to are making sure that there aren't any surgical scars that didn't already come up when we were talking about her surgical history. 00:19 We might also be looking for any signs of purple striae, which could be an indication of Cushing's disease. 00:24 Oftentimes, we'll miss if right underneath the belt line here, there could oftentimes be a scar from a prior cesarean section that just wasn't mentioned thus far. 00:32 So these are all the kinds of things that I'd be looking for in the abdomen. 00:36 In addition, while rare, patients with hemorrhagic pancreatitis or other causes of intraperitoneal bleeding, may have evidence of a Cullen's sign, which is hemorrhage or ecchymosis around the umbilicus versus the Grey Turner sign, which would be some ecchymosis or evidence of a prior bleed over in the flanks. 00:56 Again, those are fairly rare, but there are things to look for. 01:00 And lastly, when it comes to inspection, you know, patients who have obesity versus patients who have cirrhosis with a lot of ascites, the abdomen is similar and can be difficult to tease them apart. 01:12 But just on gross inspection, typically, a patient with a large volume ascites water is much heavier than fat. 01:19 So a person with significant ascites will have bulging flanks, that is the protuberance of the belly really pushes out to the sides, as opposed to with abdominal obesity, it tends to be more centrally mounted, so to speak. 01:33 Though of course, that's not an exquisitely sensitive or specific finding. 01:40 Next, we can move on to auscultation. 01:42 It's important to auscultate before you start pushing around on the belly, because you can certainly get those bowels fired up if you're palpating, before auscultating. 01:50 So, I tend to auscultate first. 01:54 And, you know, the teaching is that we auscultate in all four quadrants. 01:58 But keep in mind that it is impossible to localize where particular sounds are coming from in the belly. 02:03 I think auscultating four quadrants just ensures that we've listened for a sufficient amount of time. 02:08 But don't be led astray to believe that hearing some percolation over in this area means that there's some disease up in the splenic flexure. 02:17 It's just there's no meaningful data gathered in that particular way. 02:21 So auscultating, and we're going to characterize whether there's hyperdynamic, or increased bowel sounds versus decreased bowel sounds, versus absent bowel sounds, or borborygmi, is that stomach growling sound that would be characteristic of somebody who's hungry, versus the tinkling sound of a high pitched sound of almost like rainwater would be concerning potentially for an ileus, or small bowel obstruction. 02:49 Lastly, we can listen over the great vessels of the abdomen and attempt to listen for any bruits in those areas. 02:56 It's important to remember that the aorta is going to come down here from the epigastrium, it comes down here to the umbilicus were bifurcates into your two common iliac vessels that are then, of course, going to end up going into your external iliac, and your internal iliac, can form the femoral arteries. 03:14 In addition, you've got your renal vessels here. 03:16 So, it's useful to just listen quietly right over the aorta to see if you can appreciate a bruit in that location. 03:25 And then down here over the iliacs. 03:29 And then you can listen over the renal arteries as well. 03:32 Evidence of a bruit in those locations would of course, go along with atherosclerotic disease more generally. 03:41 Next up, we'll move on to percussion. 03:44 So we've already talked previously during the pulmonary exam about the benefits of percussion and how to perform it, so we'll sort of just dive in now. 03:52 It's expected when you're percussing the abdomen, to have some areas of tympany, which again, tympany is that drum like sound with a single pitch and areas of dullness because if the person's eating, there's going to be stool somewhere in the intestines so you're going to be percussing areas of dullness in those locations. 04:13 Whereas elsewhere, you'll have pockets of air filled intestines. 04:16 So, it's normal to have what's called scattered tympany. 04:19 That's what you'd expect. 04:21 It's when the entire abdomen is somewhat distended and there's diffuse tympany, that's when we start to worry about something like a small bowel obstruction with dramatically dilated bowels. 04:33 So just percussing around the whole area. 04:35 I hear dullness. 04:37 A little bit of tympany. 04:39 A little bit of mixed dullness and tympany. 04:42 Clearly, there's tympany there, that's from an empty stomach. 04:46 It's tympany over here, across the transverse colon, heading into dullness. 04:51 And then of course down here at the flanks. 04:53 It's expected that we're going to have dullness down there as we start to head towards the retroperitoneal organs. 04:58 So having talked generally about percussion in the abdomen, we're now going to attempt to percuss out the specific organs in an effort to detect any organomegaly. 05:07 We'll start off by percussing out the liver. 05:10 Clinicians in general aren't great at determining liver size. 05:14 But nonetheless, this is a skill that's worth developing. 05:18 So the liver is typically between 6 to 8 centimeters in size, and it's going to be maybe a centimeter or two below the costal margin, and then rising up towards the cephalad, essentially. 05:32 So, I'm going to start percussing up here over the resonant area of her lungs, which is resonant. 05:43 And right there is where I get some dullness. 05:46 Keep in mind that as she's inhaling and exhaling, the diaphragm is of course moving up and down with tidal volumes. 05:53 So the upper border of the liver is actually dynamic itself, unless, I were to have her hold her breath. 05:58 but I'm comfortable that the top of the liver is around here. 06:01 So, now we'll go to the bottom of the liver. 06:03 I'm going to displace her breast cephalad, and start here. 06:07 Again, I'm over the liver still. 06:12 And right there, you can start to hear some tympany, as I start to head towards her transverse colon. 06:20 It's clearly resonant there, or tympanic right there. 06:24 So, we know that her liver span is approximately from around here to here, which again is around 6 centimeters, which would be normal. 06:31 Similarly, with the spleen, we can attempt to percuss out the spleen. 06:35 In general, when we're talking about trying to assess splenomegaly. 06:38 We use a specific area called Traube's space. 06:41 I'm going to again, displaced your breast cephalad. Great. 06:45 And Traube's space is a triangle that's demarcated by the 6th rib here. 06:51 The lower costal margin, which is here, and then the anterior axillary line. 06:58 So you can see that's a triangle formed there, and that's Traube's space. 07:02 Now, in general, Traube's space is right over the stomach. 07:04 So it should be tympanic. 07:06 Which it certainly is. 07:08 If a patient has significant splenomegaly, the spleen typically enlarges, medially, medially, and anteriorly. 07:16 So it can displace the stomach and you end up with dullness in that area. 07:21 The most sensitive and specific part of Traube's space is a specific location called Castell's point, and that is essentially this corner of the triangle, down here. 07:32 This is called Castell's point. 07:34 And again, it's around the infracostal, the lower costal margin, and the anterior axillary line. 07:40 So I'm going to percuss there. 07:42 And you can see there's tympany over that area. 07:45 And now, what I'm going to have you do, Shayla, is take a deep breath, please. 07:51 Still tympanic, a little bit less tympanic, but definitely still tympanic. 07:58 When somebody Castell's point becomes fully dull during inspiration, during, you know, when you inspire the diaphragm is coming down, and it's pushing the spleen along with it, that would be a potential marker for splenomegaly. 08:12 So, that being said, well, Castell's point is perhaps the most useful part of assessing spleen size turns out that none of the assessments of spleen size at the bedside are particularly great. 08:24 So, while it may support that diagnosis, you can't hang your hat on it, just based on whether it's present or absent. 08:30 But nonetheless, that's how you assess for Castell's point. 08:34 So having now completed percussion, we can move on with palpation. 08:38 We're going to focus when we're doing palpation on a patient who's not having abdominal pain. 08:43 We're going to come to assessing the painful abdomen later on. 08:47 But let's start off with just doing palpation, and in a person who's not complaining of pain. 08:51 So, first off, it's always good to remind ourselves of the quadrants of the abdomen. 08:56 There's two different systems for identifying different regions in the abdomen. 09:00 The simplest one is simply dividing the abdomen to four quadrants. 09:04 Upper left, lower left, upper right, lower right. 09:08 And depending upon which quadrant we're talking about, there are certain diseases associated with each side. 09:13 So, your left lower quadrant, you're thinking about things like diverticulitis or ovarian torsion, ovarian cysts, etc. 09:21 Up here, in the top left, we're thinking about diseases of the spleen. 09:25 Of course, you're bordering with the stomach area as well. 09:29 Up here in the upper right, you're thinking about things like liver abscesses, but more likely you're thinking about cholecystitis and then down here in the right lower quadrant, for example, appendicitis or again, ovarian pathology. 09:42 That's a quick broad overview of the different kinds of things we're looking for. 09:46 When I start off examining the abdomen, I'm doing light palpation first, just simply, I'm going to lightly push on your belly here. 09:55 And you're just basically trying to make sure the patient doesn't have exquisite tenderness anywhere. 09:59 You also don't want to start over a patient by diving deep into their retroperitoneal space right off the bat. 10:06 So this gives them a chance to relax their abdominal musculature, so you can actually get in there and really try and feel things in more detail. 10:14 Sometimes it's useful if you have a tensor abdomen to have the patient flex their hips a little bit. 10:20 I'm just going to do that for purposes to demonstrate now, just like that. 10:23 I think it's uncomfortable if sometimes for patients to stay in this position because your ankle is so plantar flexed. 10:28 But if you're trying to relax the abdomen, that's one strategy to do that. 10:31 You can put your feet down again, Shayla. 10:35 So with that in mind, I'm now going into deeper palpation. 10:47 And then returning to organomegaly, we're going to attempt to complement our percussion by using palpation to find these specific organs. 10:56 So for the liver exam, there's many different approaches that have been described. 10:59 The hook method can work pretty well. 11:01 You want to start all the way down by the umbilicus. 11:03 So you don't want to start right on top of the ribs because you could be confused. 11:07 So, I'm starting here at the umbilicus. 11:10 And I'm just slowly heading proximately. 11:13 The finger pads of your fingers are the most sensitive in terms of the density of receptors there. 11:19 So, rather than using your fingertips, you want to have your finger pads aligned towards the organ that you're trying to palpate. 11:27 And keep in mind that the liver tends to enlarge medially as well as inferiorly. 11:33 So you may find that the lateral or the medial lobe of the liver is right here in the epigastrium. 11:39 Are you okay? And so, I can feel her liver edge, and it's smooth, and it's soft. 11:55 Sometimes you can buoy the liver by pushing down in this sort of way. 11:58 You can sort of feel it coming back up to your fingertips. 12:01 And it's normal to have the liver be again, 2 centimeters below the costal margin. 12:08 While clinicians aren't great at assessing liver size, as I said before, it turns out that the firmness of the liver, if you appreciate a firm liver edge beneath the costal margin that can be supportive of the diagnosis of cirrhosis. 12:23 So that's it for her liver. 12:24 Moving on to the spleen, I'm going to come around to the other side of the table. 12:30 This is called the hook method, where you're basically against starting down by the umbilicus, and marching towards the left costal margin. 12:43 And I'm hooking underneath her rib cage to try and find her spleen. 12:49 While you may find a spleen on some people, it's actually more common to not be able to palpate the spleen. 12:55 And I am not able to palpate her spleen. 12:58 So, that's not unusual. 13:08 And the last thing that we want to palpate, especially in older patients with a history of smoking is to see if there's any evidence of an abdominal aortic aneurysm. 13:17 So, again, the aorta is going to lie here between the epigastrium and the umbilicus. 13:21 So I'm just putting my fingers down here in this area. 13:28 It's normal to feel the aorta, of course, especially in a thin person, but what you're trying to distinguish is the borders of the aorta. 13:38 If you can feel a pulsatile, expansile mass in the abdomen that's greater than 3 centimeters, there's a high likelihood that, that patient does have a abdominal aortic aneurysm, which would of course, then be followed up by an ultrasound. 13:57 And her aorta feels completely normal. 13:59 Again, probably two centimeters, no more than three, which is normal to be less than two centimeters. 14:08 I did mention that there's two different schematics for assessing the different quadrants in the abdomen. 14:13 And I'll just mention the last strategy as well. 14:16 The other strategy is divided into nine segments, with the hypochondriac areas appear right underneath the ribs. 14:24 That's what hypochondriac means. It's underneath the ribs. 14:28 And in fact, in antiquity, hypochondriasis or hypochondriacs were folks who constantly complained of pain under the ribs. 14:37 And nothing was ever found in those areas. 14:39 And so we started to call people hypochondriacs, if they had a myriad of complaints for which no diagnosis was found. 14:46 This is just the lateral lumbar region. 14:49 And then down here is the inguinal regions. 14:51 And in the middle is the epigastric, the periumbilical, and in the suprapubic region of the abdomen. 14:57 Lastly, you may want to palpate or even percuss the costophrenic angles in folks with concern for pyelonephritis. 15:06 Would you mind sitting up for me for a moment, Shayla? So, once the patient is sitting upright, you can sort of palpate the areas. 15:15 Again, this is the costovertebral angle. 15:18 And if there's no significant tenderness just by palpation, then you can go on and do a quick percussion. 15:24 This is again, a tool used to assess for pyelonephritis. 15:28 So, having completed palpation, we can now move on to talk about some specific conditions that we want to be able to assess in patients with abdominal discomfort. 15:39 So, now we're going to review a few specific conditions in how to identify them. 15:43 Quick simple one right upfront, in terms of palpation it's rare, but it's something to look for is a Sister Mary Joseph node, which is actually tumorous nodules around the umbilicus associated with gastric cancer. 15:57 And that was described in the early 1900s by a nurse, who discovered in this when she was working scrubbing into surgeries with a surgeon, who was resected gastric cancers and found that there was these lymph nodes all around the umbilicus and ultimately this finding was named after her, Sister Mary Joseph.
About the Lecture
The lecture Examination of the Abdomen by Stephen Holt, MD, MS is from the course Examination of the Abdominal Region.
Included Quiz Questions
Which of the following is a possible finding on visual inspection alone of the abdomen?
- Striae due to Cushing disease
- Abdominal bruits due to aneurysm
- Tenderness in the right upper quadrant
- Pain in the epigastric region
- Renal mass
Which statement is TRUE regarding percussion of the abdomen?
- Dullness is noted over solid organs and tympani is noted over air in the bowels.
- Diffuse tympani of the abdomen is normal.
- Tympani or resonance is found with percussion over the liver.
- Castell point is useful in assessing liver size.
- Dullness is noted over air in the bowels.
During palpation of the abdomen, which maneuver may be part of an appropriate exam?
- Flex at the hips and bend the knees slightly to relax the abdominal musculature
- Start with deep palpation before percussion
- Start with the area of pain first
- Expose the entire abdomen and chest before performing an abdominal exam
- Avoid looking at the patient's face during the abdominal examination
Which area of palpation is most important to assess the liver size?
- Right upper quadrant
- Left upper quadrant
- Right lower quadrant
- Left lower quadrant
- Epigastric area
Which area of palpation is most important to assess the spleen?
- Left upper quadrant
- Right upper quadrant
- Right lower quadrant
- Left lower quadrant
- Epigastric area
Which area(s) of palpation is/are most important to assess for possible aortic aneurysm?
- Periumbilical and epigastric areas
- Left lower quadrant
- Right lower quadrant
- Chest wall
- Abdominal aneurysm unable to be assessed for on palpation
Where is a Sister Mary Joseph node found?
- A palpable lymph node in the umbilical area
- A palpable lymph node in the groin
- A palpable lymph node in the axilla
- A palpable lymph node in the neck
- A palpable mass on pelvic examination
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Its one of the best Examination Demonstration I've ever seen. Perfect Lecture and a Great Professor and I like his Teaching Method.
2 customer reviews without text
2 user review without text