Playlist
Show Playlist
Hide Playlist
Erythema Multiforme, Stevens-Johnson Syndrome, and Toxic Epidermal Necrolysis
-
Slides Cutaneous Drug Reactions.pdf
-
Reference List Dermatology.pdf
-
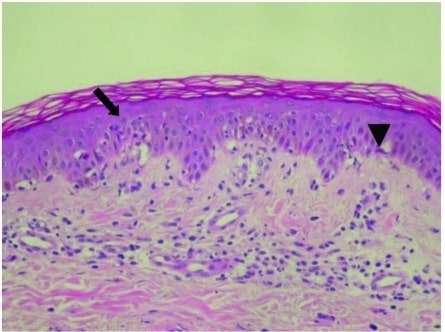
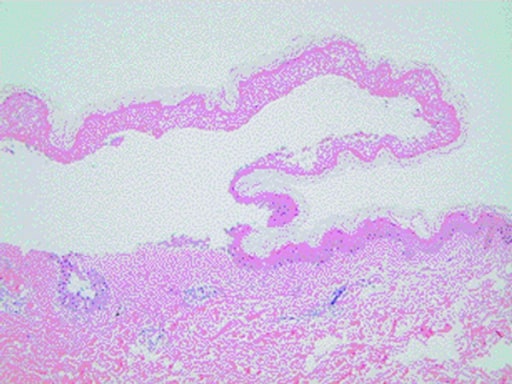
Download Lecture Overview
00:01 So reflecting back on our patient, the speed of the illness actually kind of makes sense. It's been over 1-2 days, which would be typical for toxic shock syndrome. However, we're not given anywhere in the story any obvious source of a staphylococcal infection. 00:16 Moreover, the skin findings our patient is experiencing seem more specific than the nondescript diffuse erythrodermic rash of staphylococcal toxic shock syndrome. So, while we could go and look for occult infection somewhere, I think it's reasonable to take that one off our list. 00:31 So now, let's revisit Stevens-Johnson syndrome, erythema multiforme, and toxic epidermal necrolysis. These diseases represent a spectrum of mucocutaneous drug reactions. 00:42 So let's start with erythema multiforme. Remember, the characteristic features of this condition are that it doesn't manifest with systemic symptoms, certainly not the minor variant. 00:51 And you also will have no mucosal symptoms. In contrast, Stevens-Johnson syndrome is more severe, you will have systemic features and mucosal symptoms, but you'll only have about 10% or less of the skin being involved. 01:05 The worst case scenario is toxic epidermal necrolysis. 01:09 This also has systemic features, mucosal symptoms, but more than 30% of the skin is involved. 01:15 Now, erythema multiforme, as I alluded to, has 2 different types. There's a minor variant and then a major variant, both of which are very commonly seen with herpes simplex virus. The etiology about 80% of the time is by HSV. 01:29 You can have other medications can cause it, other infections can cause it, but you're going to be looking for HSV. On the other side of the spectrum, TEN is more likely to be caused by drugs. 01:39 90% of the time it's caused by medications. Less commonly, would be infections like HSV. And Stevens- Johnson syndrome is somewhere in the middle. 01:49 E multiforme has the minor variant with no systemic symptoms, no mucosal symptoms. Then you have E multiforme major, which does have the beginnings of systemic symptoms and mucosal symptoms, but it's not quite as severe as Stevens-Johnson syndrome. 02:03 Between that 10% and 30% window of skin involvement, we have what's called the SJS/TEN overlap syndrome. 02:10 So, as a quick aside, I want to highlight that while I've put E multiforme and TEN on the same continuous spectrum, it's important to realize that they're actually actually considered separate diseases, rather than a mild and a more severe form of the same disease. 02:24 All right. So, looking a little bit more at erythema multiforme, this is an acute, immune- mediated eruption with classic targetoid-shaped lesions. 02:35 You're going to see it mostly in young adults under the age of 30. 02:38 And again, 90% of the time it's caused by infections, most notably HSV and mycoplasma. Less commonly, as I said, it's going to be caused by medications. 02:48 The classic lesions are targetoid erythematous papules that are symmetrically distributed on the hands and the face, with a centripetal spread to the torso. Remember, centrifugal and centripetal. 03:00 It can be hard to remember these 2 different terms. Centrifugal has "fug" in it, which makes me think of the root word for fugitive. 03:06 Fugitive is running away. So, centrifugal means going away from the body out to the periphery, where centripetal means coming from the periphery back into the body. 03:16 We mentioned there's a minor and a major subtype, the difference being that major subtypes are going to have more systemic manifestations and potentially, mucocutaneous involvement. 03:25 And lastly, to treat it, you're going to mostly provide supportive care for this self-limited illness, with topical or systemic glucocorticoids for more severe presentations. 03:35 While it's important to identify and withdraw any potential culprit medications, treatment of HSV is rarely indicated as EM typically presents too late in the course of an HSV flare for antivirals to be effective. 03:47 Next up, let's talk a bit more about the SJS-TEN spectrum. This is a T cell-mediated on keratinocytes. 03:55 As we mentioned, the usual cause of SJS and TEN is medications, especially as you get more towards the TEN side of the spectrum. 04:04 At least 70% for SJS and closer to 90% of TEN will be caused by medications. And then you've got mycoplasma and potentially, HSV. The culprit medications most commonly are anticonvulsants, sulfonamides, allopurinol, penicillin, and NSAIDs. So these patients are going to present with fever, myalgias, and malaise, and they're going to have a rash that begins with erythematous macules that rapidly progress to erythroderma, and ultimately, bullae formation. And this is indicative of epidermal necrosis. 04:35 You're going to have a positive Nikolsky sign because this lesion is happening with the bonds between keratinocytes, so you can simply rub your thumb on the skin and you'll see the skin slough off. 04:46 90% of such patients have mucosal involvement, which again is going to distinguish it from erythema multiforme minor. 04:53 And this can involve the oral mucosa, the lips, the conjunctiva, and the genitalia. 04:58 There is high morbidity and mortality associated with this condition. As you might imagine, all of that skin being sloughed off means your immune barriers are not working. You've got infections that can happen, all these electrolytic imbalances, hypovolemia, and of course, you can get septic shock, as well. Because of that the mortality ranges between 10%-50% for patients with TEN. 05:19 Many weeks later is when re-epithelialization can occur, and so you've got several weeks of this pruritive immune dysfunction, where you're susceptible to infections and all these electrolyte imbalances. 05:30 Last comment I would make thinking back to our patient is that patients with HIV are 100 times more likely to develop SJS and TEN. 05:40 Okay, with all that in mind, let's revisit our case. 05:44 Well, as I just said, HIV positivity is a significant risk factor for SJS and TEN. Other risk factors would include having an active cancer. 05:53 His features with fever, muscle aches, and a rash, the quick onset, these things really do lean us towards thinking about SJS and TEN. The skin was tender to the touch. 06:05 Tender skin would be a characteristic feature, again, of SJS and TEN. The throat being sore may just be indicative of early mucosal involvement. 06:14 The fact that he also has his eyes burning would suggest conjunctival involvement. 06:18 And look at this, allopurinol. This is one of those common culprit drugs that can cause this cutaneous, mucocutaneous drug reaction. The time course, actually, is about right. 06:31 The typical time course can be between 4-28 days after drug exposure, and he's had about 9 days since starting allopurinol. 06:39 And then back to the physical exam, I'll just draw your attention to the words in bold. 06:43 It covered 40% of the total body surface. 06:48 Well, recalling the 1 distinction between SJS and TEN, that 30% number, since he has 40% involvement, we can say, with confidence, that our patient has toxic epidermal necrolysis. This is potentially very bad news. So let's talk about the management. 07:06 Well, you can guess the first step is going to be to stop the allopurinol. 07:10 You're going to admit this person to the ICU, both by virtue of all of these skin manifestations and the potential for all the systemic involvement features, as well. 07:19 You're going to provide supportive care, IV fluids to help with all his electrolyte imbalances, wound care to promote healing and minimize infections analgesics, this can be an extraordinarily painful condition. 07:30 You also want to maintain his nutrition status since he may have difficulty swallowing foods. 07:34 IV glucocorticoids have been shown to be somewhat effective, but there's debate about its use, knowing that that can be further immunosuppressant. 07:42 IVIG may be helpful and cyclosporine has also been studied. 07:46 All right. Having covered erythema multiforme, SJS, TEN, staphylococcal toxic shock syndrome, and pemphigus vulgaris, we're going to quickly now take a look at a few other common adverse cutaneous drug reactions that you're likely to encounter. 08:01 We like to break these into 2 broad categories: the non-immune mediated, and the immune-mediated.
About the Lecture
The lecture Erythema Multiforme, Stevens-Johnson Syndrome, and Toxic Epidermal Necrolysis by Stephen Holt, MD, MS is from the course Allergic and Immune-mediated Skin Disorders.
Included Quiz Questions
Which of the following is true of erythema multiforme minor?
- It is associated with targetoid-shaped erythematous lesions.
- It is associated with systemic symptoms and mucosal involvement.
- Antiepileptics are the most commonly identified precipitant.
- It involves 10–30% of the total body surface area.
- Lesions tend to move away from the center.
Which of the following complications is associated with Stevens-Johnson syndrome/toxic epidermal necrolysis?
- Septic shock
- Volume overload
- Positive nitrogen balance
- Obstructive shock
Which of the following is true of toxic epidermal necrolysis?
- Re-epithelialization requires several weeks.
- It involves 10–30% of the total body surface area.
- HSV is the most common precipitating factor.
- It is associated with immune-mediated destruction of the dermoepidermal junction.
- Tender erythematous macules progress to tense bullae.
Which of the following medications is associated with Stevens-Johnson syndrome?
- Allopurinol
- Prednisolone
- Rituximab
- Cyclosporine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
lecturio help improved knownlegde and allow attendent to kerp with update