Playlist
Show Playlist
Hide Playlist
Dyspepsia with Case
-
Slides Gastroenterology 04 Nausea Vomiting.pdf
-
Reference List Gastroenterology.pdf
-
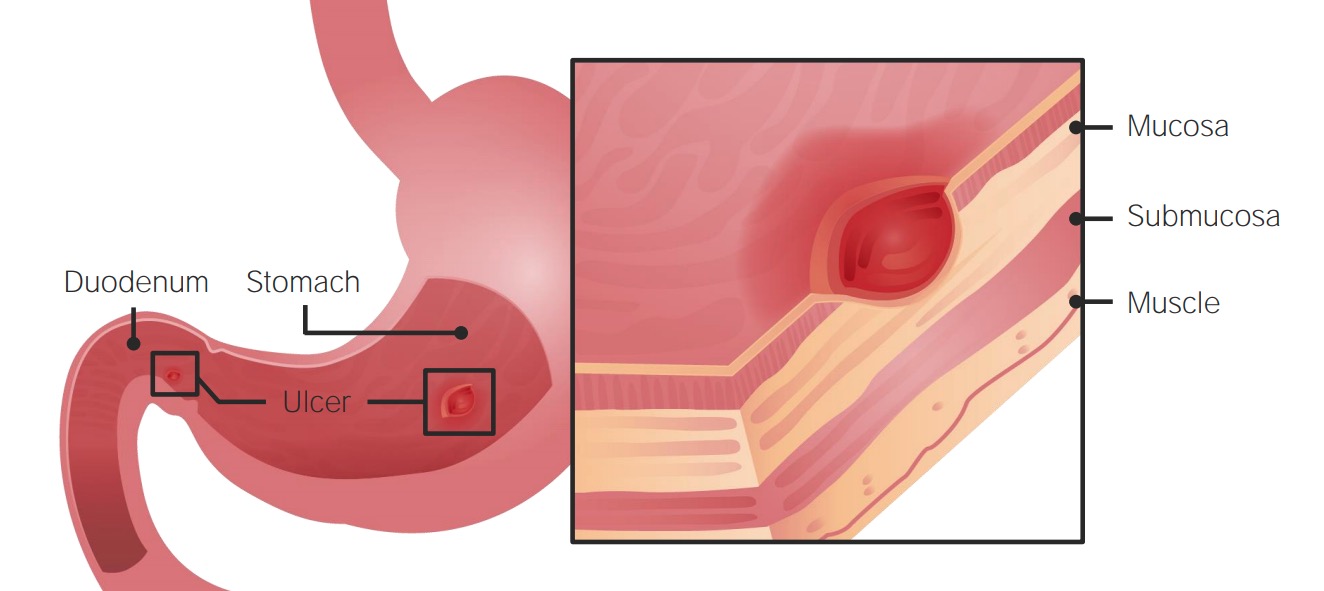
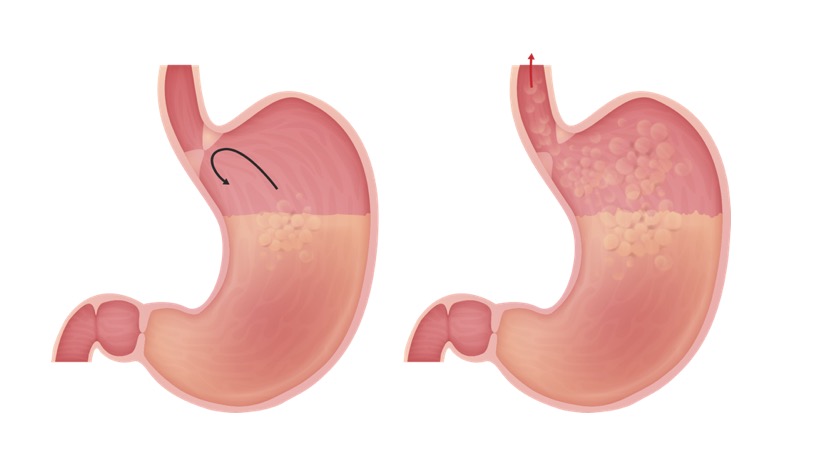
Download Lecture Overview
00:00 Today we'll talk about the approach to the patient with nausea and vomiting. 00:05 We'll begin with the definition. 00:07 So what is dyspepsia? Dyspepsia is a clinical term that we use to refer to a constellation of symptoms that includes gastric, epigastric pain or burning, abdominal bloating and nausea and vomiting. 00:21 So now let's begin with a case. 00:23 We have a 53-year-old woman seen in clinic for 8 months of epigastric pain. 00:27 Her pain is intermittent, described as a sense of abdominal bloating and discomfort. 00:33 Her symptoms tend to occur after meals. 00:35 She has nausea, occasional vomiting, and has lost 5 kg in the last year. 00:41 Her mother had a history of stomach cancer. 00:44 Her vitals are normal. 00:46 On exam, she has mild tenderness in the epigastric region but no palpable masses. 00:51 Her labs show a hemoglobin of 11.5 So what is the best next step in management? Let's identify some key features of this case She has chronic abdominal discomfort, nausea, vomiting and weight loss and a family history of an upper GI malignancy which is concerning. 01:12 So let's talk a bit more about dyspepsia. 01:15 Two-thirds of all cases of dyspepsia are caused by what is called functional dyspepsia which is when there is no structural or obvious etiology for the patient’s symptoms. 01:25 However, as with all functional disorders, this is a diagnosis of exclusion. 01:30 So you want to also make sure that you rule out many of the other causes that can lead to dyspepsia I'm not gonna go through all of them here, but they're here for your reference. 01:39 Note that anything from gastroesophageal reflux disease or GERD to cancer to even medications can lead to dyspepsia. 01:50 So, this brings us to the alarm features that you should always make sure to elicit for your patients. 01:56 If they have the symptoms that onset after the 50, that could be highly concerning. 02:01 They have anemia, dysphagia or odynophagia - that's difficulty with swallowing or pain with swallowing, any unintentional weight loss, a family or personal history of an upper GI cancer, a personal history of peptic ulcer disease or PUD, and any prior gastric surgeries. 02:23 If any of these risk factors are present, you should refer this patient for endoscopy Functional dyspepsia, since this is a diagnosis of exclusion has a very strict diagnostic criteria. 02:34 Symptoms have to be present consistently for the past 3 months and they have to have begun at least 6 months prior. 02:41 You must have one or more of the following features: Either postprandial fullness, early satiety, epigastric pain or epigastric burning. 02:51 Also, you must make sure there is no structural disease to explain these symptoms So we don't know what exactly causes functional dyspepsia. 03:01 It has an unknown mechanism but we suspect there are contributions for many factors including abnormal upper GI motor activity, psychological factors, genetic factors, disruption in the brain-gut interactions and disruptions in the gut microbiome. 03:19 If you are sure that your patient has no alarm features, then basic management consist of testing and treating for Helicobacter pylori infection, trialing of proton pump inhibitor or PPI, and recommending diet and lifestyle modification. 03:34 So in general, telling your patient to keep a food diary and avoid foods that are known to trigger their symptoms. 03:42 So that brings us back to our case. 03:43 a 53-year old woman who's been having chronic abdominal discomfort, nausea, vomiting and weight loss which indicates dyspepsia with alarm features and her family history of GI malignancy. 03:57 Because of the presence of all of these alarm symptoms such as her anemia, her vomiting, weight loss and her family history of GI cancer, the next step should be endoscopy.
About the Lecture
The lecture Dyspepsia with Case by Kelley Chuang, MD is from the course Approach to Patients with GI Symptoms.
Included Quiz Questions
Which of the following is the best next step in the management of dyspepsia with alarm features?
- Endoscopy
- Proton pump inhibitors
- Testing for Helicobacter pylori
- Diet and lifestyle modification
- H2 antagonists
Which of the following medical conditions is the most common cause of dyspepsia?
- Functional dyspepsia
- Gastric cancer
- Peptic ulcer disease
- Pancreatitis
- Esophageal cancer
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |