Playlist
Show Playlist
Hide Playlist
Diverticula and Hernia
-
Slides GD Esophagus.pdf
-
Download Lecture Overview
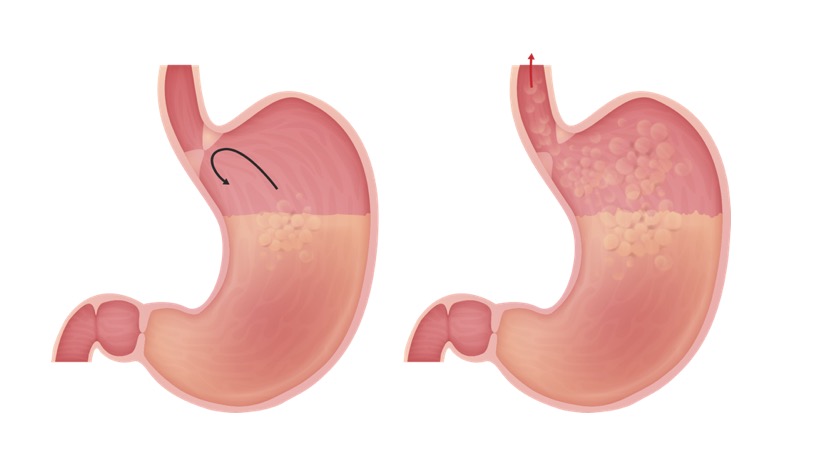
00:01 Let us now move on to Diverticulae and Hernia. 00:04 We’ll first begin with diverticulum. 00:07 So what does a diverticulum mean in general? It means an outpouching. 00:11 There’s a weakening of that particular structure in which there is an outpouching due to the pressure. 00:17 An outpouching. 00:18 Now where’s the outpouching taking place? In the esophagus, Upper Esophageal Sphincter - UES. 00:28 Can you picture that? Are you there? Good. 00:33 So now, I’m eating food. 00:36 I have an diverticulum, outpouching of the upper esophagus. 00:40 So as soon as I get my bolus down into the esophagus, where is it going? Into the diverticulum, quite a bit of it. 00:47 That’s what you expect to find on your imaging study. 00:50 There’s going to be a diverticulum in the upper portion of esophagus where it is then accumulating food. 00:55 Accumulating food. 00:57 It’s having a hard time moving obviously past that diverticulum, so it’s stuck in that pouch for a long period of time. Just like you know about your intestinal diverticulae or diverticular disease down in the intestine. That obviously will be faeces accumulating in your diverticulum. Here we have food, a bolus accumulating in the diverticulum. Either case, there it is and it’s rotting. Either the faeces, we call that faecolith, with diverticular disease of the intestine, or we have food that’s then accumulating in the upper esophagus. Upper esophagus. 01:32 If it sits and it rots, tell me about the breathe of this individual. 01:36 Woooohhoohooo! Yeah, halitosis, halitosis. 01:40 Not good. 01:41 So here once again we will have dysphagia, right? We’ll have dysphagia. 01:45 Halitosis, associated with regurgitation. Halitosis. 01:50 Imagine now the diverticulum, the body wants to get rid of the food that’s stuck in there. 01:55 Uaaagghhh, right. Regurgitation. 01:58 And treatment is surgical correction. 02:00 Surgica-... surgery, we need it because of the weakening taking place of the upper esophagus. 02:08 Let's talk about what happens when there's weakening in the diaphragm. 02:12 Allowing for parts of the GI to then enter the chest cavity. 02:18 Let's say that you're approximately at level T10. 02:22 Can you picture that for me? At T10, we have what known as esophageal hiatus with the diaphragm. 02:28 If that particular esophageal hiatus then becomes a little weaker. 02:34 We then refer to this as being hiatal hernia. 02:38 What happens here is the gastroesophageal junction and the fundus may slide into the chest cavity and if that happens may then result in loss of proper maintenance and tonicity of lower gastroesophageal sphincter. 02:54 May then predispose your patient to develop GERD. 02:59 Para-esophageal hernia means instead of esophageal hiatus through the diaphragm. 03:08 Parts of what we know or what we call the phrenoesophageal membrane which normally limits, those parts of the GI from coming into the thoracic cavity, well then become weakened. 03:22 What we usually refer to as hiatal hernia, our previous topic, often times referred to us as being Type 1. 03:31 We start getting into realm of Type 2 and Type 3 and Type 4. 03:37 Then, at the story about the para-esophageal hernia. 03:41 Let’s talk about that story. 03:43 At first, if the phrenoesophageal membrane becomes weakened then you may then have para-esophageal where herniation of the stomach next to the gastroesophageal junction, GEJ. 03:57 May then cause bleeding and then perhaps there might be strangulation infraction taking place. 04:03 As a hole gets larger then more of the stomach may then get in and by the time you get into Type 4, where we refer to us as being hernia. 04:16 It's just have the para-esophageal type the entire stomach imports even of the intestine may be found in the thoracic cavity. 04:25 It may then be seen with baruim swallow.
About the Lecture
The lecture Diverticula and Hernia by Carlo Raj, MD is from the course Esophageal Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following accurately describes the pathology of Zenker's diverticulum?
- Weakening of the mucosa of the esophagus above the upper esophageal sphincter
- Weakening of the mucosa of the esophagus near the lower esophageal sphincter
- Weakening of the submucosa near the upper end of the esophagus
- Weakening of the submucosa near the lower esophageal sphincter
- None of the above
A 35-year-old woman presents to the clinic complaining of difficulty in swallowing, regurgitation, and halitosis. What is the MOST likely treatment?
- Surgical correction of the esophagus
- Lifestyle modification
- Proton pump inhibitors
- Antacids
- All of the above
A middle-aged man presents to the urgent care clinic complaining of severe heartburn after meals. He also reports chronic chest discomfort but denies changes in appetite or difficulty swallowing. What is the MOST likely diagnosis?
- GERD
- Gastric cancer
- Esophageal stricture
- Esophageal ring
- Costochondritis
A patient with a para-esophageal hernia is at a high risk of which of the following conditions?
- Strangulation
- Ulceration
- Inflammation
- Acid reflux
- All of the above
What is the definitive treatment for a hiatal, or para-esophageal, hernia?
- Surgery
- Proton pump inhibitors
- Antacids
- Lifestyle modification
- Iron supplementation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It is a nice prasentation with a prompt accuracy and clear discription