Playlist
Show Playlist
Hide Playlist
Distal Convoluted Tubule (DCT): Bartter and Gitelman Syndrome
-
Slides DCT Pathophysiology RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
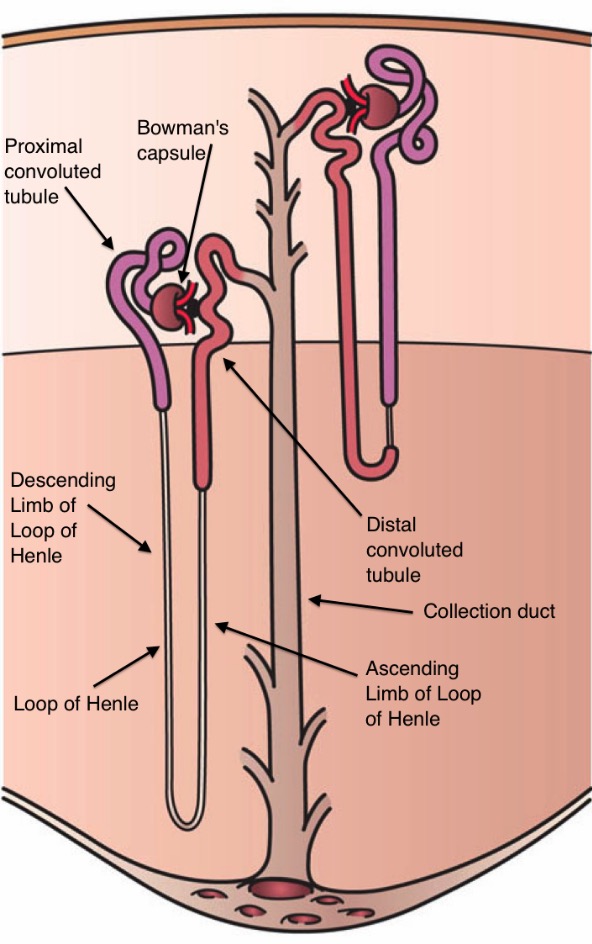
00:00 So down here. 00:02 Lets talk about this. A lot of words. Let me give you the overview. We will get into specific pathologic problems. One is called Bartter, the other one is called Gitelman, okay. Now we are going to put this together right now because I need you to at least know that these are pathologic conditions that you are mandated to know within the nephron starting from the thick ascending limb and then finally end up at the collecting duct. 00:34 The overview as far as common, distinctive and then we will get into distinctive features are going to be the following. The tubular defects in sodium chloride transport and two different places. Think about that for one second. If it is the thick ascending limb, how is the sodium being reabsorbed? Sodium- potassium-2 chloride. If it is the distal convoluted tubule, how is that sodium being reabsorbed? Sodium, chloride. Next thick ascending limb. What kind of diuretic? Loop. What about the distal convoluted tubule? What kind of diuretic? Thiazide. Next, well to make your life a little bit easier, let us now do our alphabetic order. B before G at the same time I want to go from proximal to distal in your nephron. 01:24 The loop diuretic, which would be a problem with the sodium-potassium-2 chloride that pathology is called Bartter.You see what it says loop diuretic mimicking Bartter syndrome. 01:36 Stop there. Where are you? Thick ascending limb. It behaves like a loop diuretic. You tell me now the pathology for Bartter syndrome is dealing with which sodium channel? Sodium- potassium-2 chloride. Are we done? Not at all. I have to give you clinical manifestations, then I must give you the genes. 01:57 Next, I want you to go distal convoluted tubule. What was the name of that sodium channel? Sodium chloride is thiazide-sensitive. Right. So, therefore, this will be Gitelman. What is the next letter? G. Gitelman is like a thiazide drug. These are pathologies that mimic the pharmacologic agents in terms of how you want to approach this. 02:20 Next, impaired sodium chloride reabsorption leads to mild volume depletion, hypotension thus what does it activate? Highlight highlight highlight RAAS. Next the combination of, why do we call the secondary hyperaldosteronism, why? Why? If you are losing fluid, then what are you going to release? Renin, how? Secondarily. 02:46 When you have volume depletion, this is going to be secondary hyperaldosteronism. 02:52 Walk through this further. Where does aldosterone work? It works in the distal convoluted tubule. 02:57 What is it going to do? You see the bolden words there. That is the key. Normal physio. 03:03 Aldosterone works to do what? To get rid of potassium. You are at risk for hypokalemia. 03:08 What are you worried about with hypokalemia please? The more that you get rid of the potassium, the more that you have hypokalemia. Think about your resting membrane potential, the resting membrane potential is going to become more negative right. It is going to become hyperpolarized, more negative. Meaning that it's further way from what? Further way from threshold. What kind of issues might you have? You have issues with the heart obviously, and you have issues with skeletal muscle, fatigue. Next, aldosterone gets rid of your hydrogen result in metabolic alkalosis respectively. Move on. Okay now. Point by point by point, we are going to walk through this so that we talked about the overview. Now we are going to give you some distinctive feature for each disease so that you will quickly be able to figure this out. In the meantime, Bartter, Bartter, Bartter. Reflexibly where is my problem? Thick ascending limb, sodium-potassium- 2 chloride. Gitelman syndrome, where are you? Distal convoluted tubule and behaves like a thiazide drug meaning sodium chloride channel. 04:14 Keep repeating that over and over again. Lay down the foundation. Now come back here. Patients in both conditions have suppressed activity of ADH why? Due to physiologic loss of renal diluting capacity really. The fact that ADH isn't working properly is why? I told you earlier about that kind of countercurrent mechanism. I told you that if that has been somehow impaired that you are going to lose the ability to properly concentrate and may be perhaps even, be able to properly dilute. In both conditions, please understand that the diluting ability of the nephron has been completely or severely impaired. Thus what hormone are you now influencing negatively? ADH. So ADH is going to be suppressed. Make sure you understand that in both conditions. Now, listen here. Concentrating. Remember that sodium-potassium-2 chloride. 05:16 Where? Thick ascending limb and what is that called when you have the thick ascending limb that communicates with the descending limb. The two loops or ends of the loops are communicating with one other. Can I help you? Is what the thick ascending limb is asking the descending limb? The descending limb says yes actually I do. I do need a little bit of help. What might I want to give you? How about some solute so I can give you some water. Oh! Yes, I can give that to you. So thick ascending limb provide the sodium-potassium-2 chloride. 05:52 There it is. Put to the interstitium creates an osmotic gradient so that water can come out. Simple. What is this? Countercurrent mechanism. What is this? The concentrating ability. Where is my concentrating ability? Down in the loop. Right? Are you with me? So if you haven't understood the physio how in the world is the pathology going to come in to play? How are we going to make sense of this? So we now got the sodium-potassium-2 chloride, What ability are you losing? Good. The concentrating ability. Relatively spared in Gitelman. How come? Where is Gitelman? Good. Distal convoluted tubule. What's over there. 06:30 It is a thiazide-sensitive sodium chloride. Does that really participate in concentrating ability? No. More so diluting. I will give you that. But concentrating? Border. Much more slow, much more slow. In both conditions, though. What about ADH? Suppressed. Take a look at the previous bullet point. Good. Pay attention to this one, because this is a distinguishing feature. Another big one. Urinary calcium excretion. Take a look. Stop. Pay attention. 07:02 Hypercalciuria. Take a look at the suffix. Uria. So where is there more calcium right now? In the urine. Are we okay now? Okay. What is happening? If you knock out that sodium- potassium-2 chloride, are you able to properly take up your calcium? No. Remember the back leak. Remember that. What was the name of that receptor? ROMK. Good. So if you don't have proper functioning of that ROMK with back leak because the sodium-potassium-2 chloride channel has been knocked out due to Bartter, how in the world are you able to properly take up your calcium? You cannot. Urinary calcium excretion is normal or high in patients with Bartter, not the case with Gitelman. Are we okay there? So that bullet point of second and third become very important for you to distinguish between Bartter versus your Gitelman.
About the Lecture
The lecture Distal Convoluted Tubule (DCT): Bartter and Gitelman Syndrome by Carlo Raj, MD is from the course Diseases of the Nephron.
Included Quiz Questions
Which of the following is a common feature in Bartter and Gitelman syndromes?
- Suppressed activity of ADH.
- Impairment of concentrating ability.
- Urinary calcium excretion is normal or high.
- NKCC channel is affected.
- DCT is the site of impairment.
Which of the following is incorrect regarding Bartter syndrome?
- Proximal convoluted tubule is the site of impairment.
- Concentrating ability is impaired.
- Urinary calcium excretion is normal or high.
- NKCC channel is affected.
- Thick ascending limb of the loop of Henle is the site of impairment.
Which of the following is correct regarding Gitelman syndrome?
- There is an impairment in the sodium chloride channel in the distal convoluted tubule.
- Concentrating ability is impaired.
- Urinary calcium excretion is normal or high.
- NKCC channel is affected.
- Thick ascending limb of the loop of Henle is the site of impairment.
Which of the following electrolyte imbalances is observed in Bartter and Gitelman syndromes?
- Hypokalemia and metabolic alkalosis.
- Hypokalemia and metabolic acidosis.
- Hyperkalemia and metabolic alkalosis.
- Hypernatremia and metabolic alkalosis.
- Hypokalemia and respiratory alkalosis.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Bravo Bien entendu, of course. The pieces slowly coming together whith each lecture. Adh chemical from brain regulating water channels TAL upstream DCT downstream concentration/dilute Salt/water Sure there is a canal chamber lock analogy here somewhere. These little grey cells.
I think that Dr Raj is simply amazing because he has the ability to make even the most intricated concepts clear and easy to understand!