Playlist
Show Playlist
Hide Playlist
Dissection of the Aorta: Symptoms
-
Slides 05 VascularMedicine advanced.pdf
-
Reference List Vascular Medicine.pdf
-
Download Lecture Overview
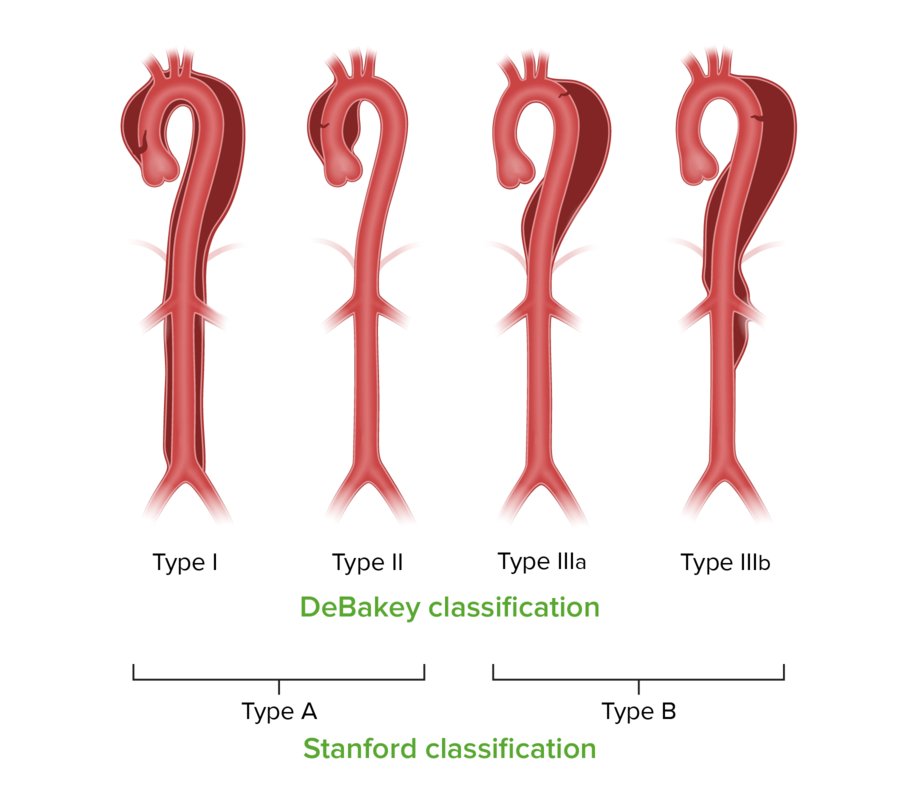
00:00 The symptoms, when a dissection develops, are usually sudden onset of severe pain. The difference between the pain of dissection and the pain of myocardial infarction or heart attack is that the pain of heart attack usually starts mild and builds, whereas the pain from dissection is maximum right at the onset. Some patients describe the pain as "tearing" or "ripping" in nature—very different from the almost dull, constant indigestion-like pain of myocardial infarction. A Type A dissection involves the ascending aorta, often extending down into the descending aorta, but the start… Dissections are named for where they start. 00:49 The aortic dissection of Type A is usually associated with severe anterior wall chest pain. Type B starts distal to the left subclavian artery—in other words, in the descending aorta—and spares the ascending aorta, and that leads the patient often to complain of severe onset of back pain. As the dissections spread, blood pressure may be diminished in certain areas, because the dissection cuts off certain blood vessels. 01:19 For example, the brachial artery can get cut off, and suddenly, the radial pulse disappears. 01:26 If the dissection extends up into the carotid arteries, the patients may present as a stroke with hemiplegia (paralysis of one side of the body) or even just partial paralysis. 01:38 And patients can present with heart failure if particularly the Type A or ascending aortic dissection extends back and causes the aortic valve to have an abnormal structure or formation because of the dissection in and around the valve ring, and that causes aortic insufficiency and can cause sudden onset of acute heart failure. Often, fatal complication of aortic dissection is if it ruptures into the pericardium. This causes pericardial constriction. The heart suddenly is being squeezed by the large volume of blood in the pericardial space. 02:17 Cardiac output drops, and the patient goes into shock and often dies. 02:22 The diagnosis, of course, just like in any other condition: It starts with a good history and physical exam, usually looking for abnormal pulses and, in addition, the character of the pain that I've just described. In order to confirm the diagnosis, you need some form of noninvasive imaging, so could be MRI, could be transesophageal echo, could be CT. In an occasional setting where you're considering putting a stent into the patient, often because you think they're high risk for full surgery, the dissection could be confirmed by aortic angiography. But almost always, a noninvasive technique is the first one. But remember, the clue is in the history and the physical examination: missing pulses and a severe pain at the moment it started, suggesting dissection. It's of interest that with a technique like MRI, we can actually produce three-dimensional images of the aorta and determine with great accuracy where the tear is, which branch vessels are involved, and locating any secondary tears where the dissection tears the intima and reenters the main channel again. This is very helpful to the surgeons and to the angioplasty folks who are going to be trying to repair this. The noninvasive technique, of course, doesn't involve the use of any contrast dye and… but it can help also to detect the amount of aortic insufficiency if the dissection has worked its way back into the aortic valve. So the MRI is very, very accurate. It just takes a little longer, and these patients are often critically ill, so they may... You may not have time for an MRI, in which case you would do a… probably a transesophageal echo. Once more, just to give you the classification of the dissections: The one in the ascending aorta, the tear usually occurs just above the aortic valve, and that's called a Type I. This classification was first utilized by Dr. Michael DeBakey, one of the pioneer cardiac surgeons at Methodist Hospital in Houston, Texas. Type I—here, you can see in the diagram—starts… The tear is just above the aortic valve, and the dissection goes all the way down into the distal abdominal aorta. A Type II is actually fairly rare. It's an ascending aortic aneurysm, but it doesn't descend... It doesn't extend down into the descending aorta. It just stays localized to the ascending aorta. That form is a little more common in patients with Marfan's syndrome, but we don't see that very often. Type III is also quite common. You see it occurs in the descending aorta, distal to the left subclavian artery, and extends down into the abdominal aorta. The Stanford has also... Stanford University has also come up with a more simplified classification for aneurysms compared to DeBakey. They just say, "Type A" and "Type B." Type A evolves… involves the ascending aorta; Type B spares the ascending aorta and is just involved… just involves the descending aorta. Regardless, each of these are potentially life-threatening, and they may be life-threatening in a relatively short period of time, so this is a medical emergency. Now, let's talk a little bit about therapy
About the Lecture
The lecture Dissection of the Aorta: Symptoms by Joseph Alpert, MD is from the course Arterial Diseases.
Included Quiz Questions
A dissection of the aorta usually causes which of the following symptoms?
- Severe chest discomfort.
- Headache.
- Severe muscle cramps.
- Uncontrollable diarrhea.
The character of pain in case of aortic dissection can be described as which of the following?
- Severe, sudden onset.
- Mild building over time.
- Recurrent.
- Mild.
- worsening on standing.
Type B aortic dissection most frequently causes pain in which of the following areas?
- Back.
- Right hand
- Anterior chest wall.
- Left hand.
- Neck
Which of the following systemic conditions is associated with type A aortic dissection?
- Marfan syndrome.
- Treacher-collin syndrome.
- Ramsay hunt syndrome.
- Posttraumatic stress disorder.
- Myelodysplastic syndrome.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |