Playlist
Show Playlist
Hide Playlist
Disease Modifying Anti Rheumatic Agents (DMARDS)
-
Slides DMARDS.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
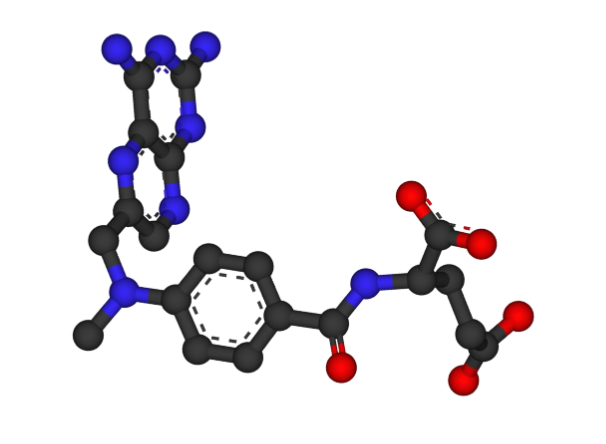
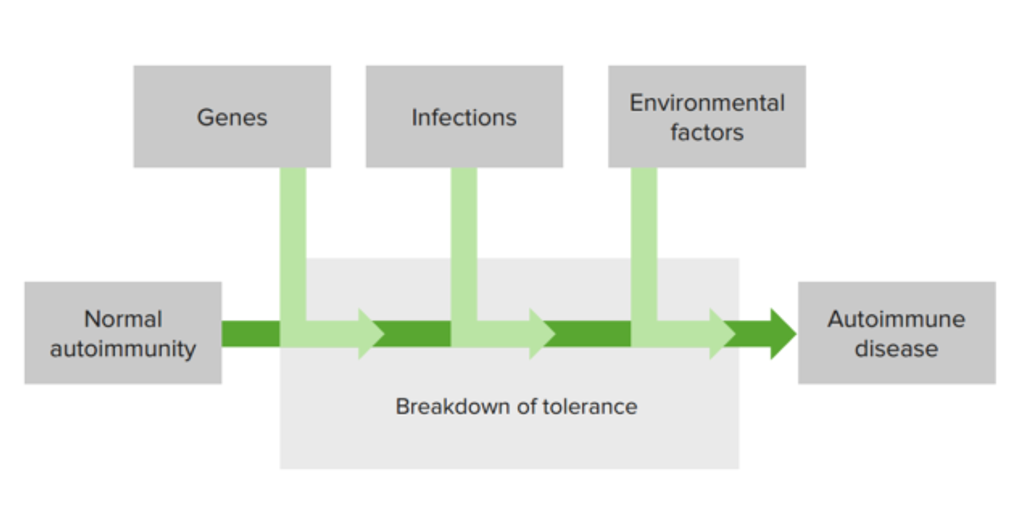
00:00 Let's move on to the disease modifying anti rheumatic agents or DMARDs. 00:05 Now remember these all drugs are cytotoxic agents. So you shouldn't just jump on the bandwagon to get people on DMARDs without any kind of experience with these drugs. 00:17 The first of them and the prototypical DMARD is methotrexate. Now we often give methotrexate once a week. 00:23 And because they also affect folic acid activity, we give it with folic acid supplementation. 00:31 This is an antifolate drug. It inhibits dihydrofolate reductase. What is that relevant? Because this reduces thymidine synthesis. Now remember thymidine is one of the agents used in DNA, so if you have less thymidine, you're going to have less expression of DNA fragments. 00:49 The primary mechanism is used in cancer chemotherapy and it limits a cancer cell from dividing because there's less DNA. 01:01 In rheumatoid arthritis, there are multiple mechanisms of action. Number 1, there is accumulation of adenosine. 01:09 Number 2, it inhibits the T cells. Number 3, it suppresses intercellular adhesion molecules of the T cells so the T cells can't attach to their target. And remember T cells are very important in inflammation. 01:24 And finally, it inhibits interleukin 1 beta binding to the cell surface receptors which is the primary mechanism of how inflammation is occuring in rheumatoid arthritis. 01:36 So, there's multiple ways that methotrexate is working in RA that make it a very effective anti-RA drug. 01:43 Methotrexate is also used in other diseases as well. 01:48 Let's move on to the T-lymphocyte agents. The most well known and I would call it the prototypical drug is sulfasalazine. 01:57 Now, sulfasalazine is metabolized to 5-ASA. And yes that is related to aspirin. 02:03 It works through an unknown mechanism and it is used extensively in Crohn's disease. 02:09 Now, we're gonna talk a lot more about sulfasalazine in our GI lecture, so hold onto your hats, we're gonna talk about that later. 02:18 Hydroxychloroquine is an antimalarial drug. It works through an unknown mechanism, possibly through a reduction of lysosome release of inflammatory factors right from the cells themselves. 02:30 I'll just say that it works quite well in rheumatoid arthritis and is often used, it does have some side effects that limit its use in some patients. 02:39 One of the most well known T-lymphocyte agents is cyclosporin. It is widely used in transplantation medicine. 02:47 And it is a very potent inhibitor of the T-lymphocyte interleukin class of hormones. 02:52 It interacts with multiple drugs. Up to 2,000 drugs may interact with cyclosporin so we have to measure cyclosporin levels quite often and be very diligent with this drug. 03:05 Cyclosporin toxicity and cyclosporin under utilization or low levels of cyclosporin have the same type of clinical presentations so sometimes it's hard to tell apart toxicity from lack of effect. 03:21 Other T-lymphocyte agents include the very difficult to pronounce leflunomide, mycophenolate, and abatacept. 03:33 Once again, you know how hard it is to pronounce these drugs so I tend to not remember them on exams. 03:39 From a practical point of view, you really need to know cyclosporin. These other drugs aren't as important. 03:46 B-lymphocyte agents include rituximab. So rituximab is amazing. It is a monoclonal antibody. 03:54 You've heard me talk about monoclonal antibodies before in other lectures. 03:57 We use this new agent in refractory cases of rheumatoid arthritis. 04:02 And it binds to something call CD20 on the B cells and it actually prevents B cell activation. 04:09 Incredibly effective agent. Very few side effects. And in some cases, we're giving these monoclonal antibody treatments for rheumatoid arthritis once every four to six months. So we're starting to see a whole new generation of treatment. 04:26 I can't even call them drugs anymore. They are more an immune modulating therapies rather than drugs. 04:32 And they don't follow the old rules of pharmacology. It's an exciting time to become a doctor and I'm really excited to see what's going to happen, not just in the next year, but can you imagine in the next 10 years how we are going to change medicine? It's very exciting. 04:46 Other macrophage agents include gold. Now gold comes in several forms with respect to the DMARDs. 04:52 There's gold sodium thiomalate or GST, aurothioglucose, and auranofin. Now auranofin does come as an oral agent and it's rarely used. 05:03 These agents in general are often give as once or twice a week injections as IM injections. 05:09 We can also use these agents in treating tuberculosis. 05:13 Now, how does it work? We believe that it inhibits prostaglandin release. 05:18 There is also something called the major histocompatibility complex, and the interactions between cells rely on these complexes. 05:26 We believe gold acts by inhibiting these interactions. We know that gold certainly reduces macrophage activity. 05:34 This brings us to the last class of the DMARDs. We call these biologics. 05:39 That's because they act biologically either acting as a monoclonal antibody or by inhibiting the actions of tumour necrosis factor alpha directly. 05:48 I won't go into the exact mechanism but once again if you look at a drug and it ends in -mab, mab stands for monoclonal antibody. The two letters before -mab refer to how much of it is human and how much of it is coming from another animal. 06:04 These agents, these biologics are changing the way that medicine is being practiced. 06:09 And I encourage you to keep up on them because over time I think that a lot of these biologic treatments are going to replace the drugs that we are learning about today. 06:19 Other interleukin inhibitor reduces immune function in rheumatoid arthritis. 06:23 These are not as commonly used at this time but I suspect that over time these interleukin active agents are also going to be replacing the drugs that we are using today.
About the Lecture
The lecture Disease Modifying Anti Rheumatic Agents (DMARDS) by Pravin Shukle, MD is from the course Inflammation Pharmacology.
Included Quiz Questions
What best describes DMARDs?
- DMARDS are cytotoxic drugs.
- DMARDS are similar to aspirin.
- DMARDS are similar to NSAIDs.
- DMARDS are similar to COX-2 inhibitors.
- DMARDS are similar to chemotherapy.
A 49-year-old woman with rheumatoid arthritis comes to the clinic. Despite taking the maximum dosage of NSAIDs, she continues to experience pain and morning stiffness, with occasional discomfort during the day. She is interested in exploring a different medication. What is the most appropriate next treatment option?
- Methotrexate
- Acetaminophen
- Indomethacin
- Ketorolac
- Unfortunately, there are no other alternatives.
What is the mechanism of action of rituximab?
- Monoclonal antibody to CD20
- Monoclonal antibody to CD19
- COX-1 inhibitor
- COX-2 inhibitor
- Inhibitor of MAP kinase
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |