Playlist
Show Playlist
Hide Playlist
Diabetic Nephropathy – Secondary Nephrotic Syndrome
-
Slides Nephrotic Syndromes.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
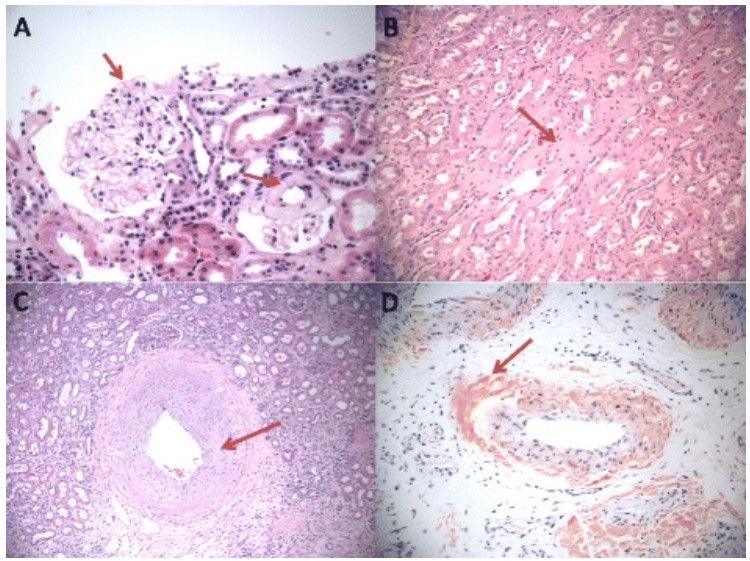
00:01 So our second disease that we talked about which was a systemic disease where podocytes are playing a prominent role but it's consequent to disease is going to be diabetic nephropathy. 00:11 This is the most common systemic illness to cause nephrotic syndrome and the most common cause of end-stage renal disease in the United States. 00:20 Nephrotic syndrome here can occur in both type 1 and type 2 diabetes mellitus. 00:25 In type 1 diabetics though they tend to have retinopathy and other forms of microvascular disease that precedes the overt nephropathy. 00:33 That same rule does not apply for our type 2 diabetics. 00:36 They can often present with nephropathy without having retinopathy and it's not uncommon for patients to come to me actually in my office with a recent diagnosis of diabetes and already manifest with nephrotic syndrome. 00:49 So when we think about the pathogenesis of diabetic nephropathy, it's really multifactorial. 00:53 There are metabolic factors that go into this things like hyperglycemia and pro inflammatory mediators that lead to an increase in synthesis of matrix proteins as well as pro fibrotic growth factors. 01:04 We also have hemodynamic factors. 01:06 Our patients are hyper filtering very at the very early onset of their disease process. 01:11 They have an increase in glomerular capillary pressure and hypertension and glomerular hypertrophy. 01:16 And finally, our patients have a genetic susceptibility. 01:21 When we think about the pathology of diabetes mellitus we can see again or normal glomerulus over here to the left, on light microscopy. 01:29 Again, I want you to notice how delicate and beautiful those capillary loops are. 01:33 Are what happens in diabetic nephropathy. 01:35 This is somebody who has advanced diabetic kidney disease and what my arrow is pointing to our diabetic nodules. 01:41 This is really a diabetic glomerulosclerosis seen on light microscopy, which is essentially the mesangial area filling up with matrix. 01:51 On EM, what I want you to notice is again, on our normally EM, we have these beautiful podocytes that are preserved in an intact, but in diabetic kidney disease, we have thickening of that basement membrane and we also have those overlying podocytes which oftentimes have foot process effacement and actually denuded areas of basement membrane because those podocytes are apoptosis in the crossing and getting picked off from the underlying basement membrane. 02:19 So how do our patients do when they have diabetic nephropathy? Early disease typically manifests with moderately increased albuminuria, what we also call microalbuminuria. 02:28 That means our patients have greater than 30 milligrams a protein in their urine. 02:33 And it may take several years to develop nephrotic range proteinuria or nephrotic syndrome. 02:36 But remember there are those cases where you can see it relatively quickly. 02:41 So when we think about treatment for our patients who have diabetes nephropathy, critical, critical for them to receive an ACE inhibitor or an ARB to reduce that glomerular capillary pressure and suppress their proteinuria. 02:53 SGLT2 inhibitors are also recommended due to their renal protective effects, including reducing intraglomerular pressure and hyperfiltration, which can help reduce proteinuria and renal function decline. 03:06 A nonsteroidal selective mineralocorticoid receptor antagonist may also be added for patients with proteinuria despite other therapies. 03:16 When they have nephrotic syndrome again, we're going to want that loop diuretic in order to mobilize that volume off their body and a low sodium diet. 03:23 We want strict blood pressure control less than 130/80. 03:27 We want to treat their hyperlipidemia and dyslipidemia. 03:29 We learned in our chronic kidney disease lecture that these patients are exquisitely sensitive and vulnerable to developing cardiovascular events. 03:37 And we want strict glycemic control. 03:39 We want those patients to have a hemoglobin A1C of less than 7%. 03:46 So remember if your patient is a diabetic even before they ever manifest with any changes, if they're hypertensive, the very first choice that we should be having for them for an antihypertensives are ACE's and ARB's. 03:59 And finally, in our patients who are type 1 diabetics, we can actually treat we can actually transplant them not only with a kidney but a pancreas so these patients can ultimately undergo a simultaneous kidney pancreas transplant and that actually is quite gratifying because we actually can cure their disease we can cure their diabetes. 04:20 So it's one of the better treatments that we have available for our patients who have type 1 diabetes. 04:26 And with that, that concludes our nephrotic syndrome lecture.
About the Lecture
The lecture Diabetic Nephropathy – Secondary Nephrotic Syndrome by Amy Sussman, MD is from the course Nephrotic Syndrome.
Included Quiz Questions
Which of the following findings on microscopy is pathognomonic for diabetic nephropathy?
- Nodular glomerulosclerosis
- Spikes and domes in the basement membrane
- Thin basement membrane
- Duplication of the basement membrane
- Focal glomerulosclerosis involving <50% of glomeruli
Which of the following is recommended to slow the progression of diabetic nephropathy?
- Decreasing intraglomerular pressure with ACE inhibitors/ARBs
- Strict glycemic control, HbA1c level of <8%
- Blood pressure control at <140/90 mm Hg
- Immune-targeted therapy
- Proteasome inhibitors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I used to mix up all the details about nephritic and nephrotic syndromes before and this is the first time it all came together and made sense. The lecture is a good mix of pathology review and clinically important info and the aesthetically pleasing slides plus the cases help a lot with memorisation. Thank you!