Playlist
Show Playlist
Hide Playlist
Defects in Acute Inflammation
-
Slides Acute and Chronic Inflammation Effector cascades.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
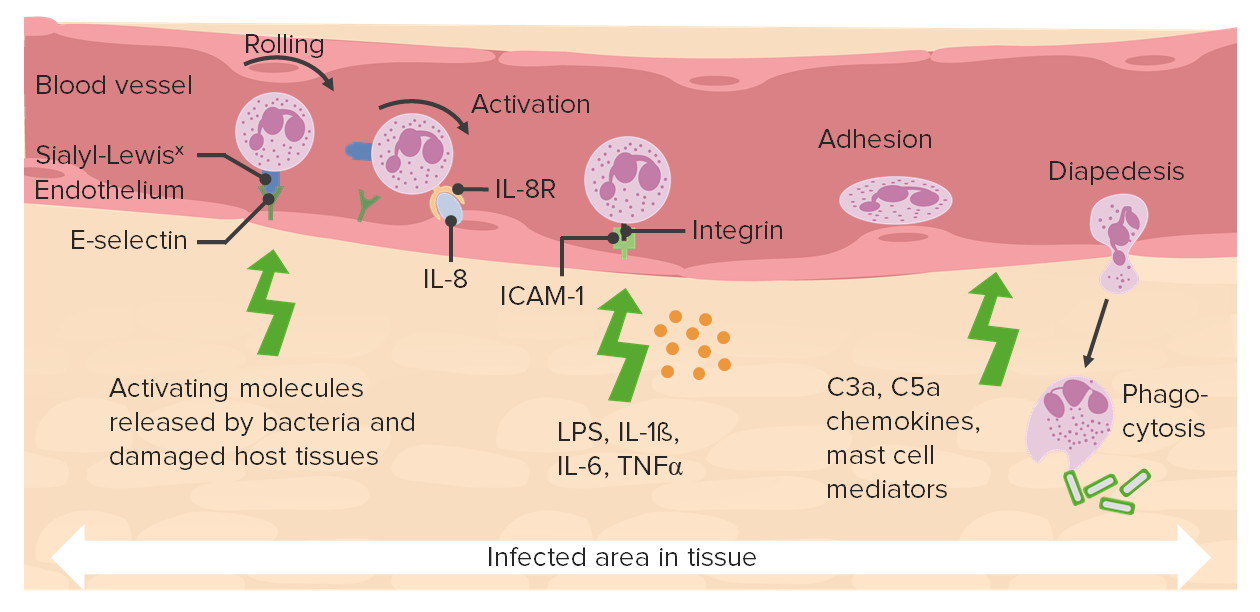
00:01 So you can have too little inflammation, you can have too much inflammation, and these will be important diseases. 00:08 So believe it or not, there are patients walking around out there not too many, but a few that have defects in the synthesis of their integrins. 00:16 So they don't bind with firm adhesion to the immunoglobulin superfamily. 00:21 As a result, they get recurrent infections. 00:24 They just don't get the cells sticking to the endothelium, so they can crawl across. 00:30 You can also have defects that lead to diminished sialyl-Lewis X. 00:34 Remember, sialyl-Lewis X is going to be that complex of sugars, that binds to our selectins. 00:42 And if we don't make the sialyl-Lewis X, we don't get rolling. 00:46 Those patients also get recurrent infections because they don't have enough acute inflammation. 00:53 You can also have defects in phagolysosome formations. 00:56 So you've eaten a bug, and you're getting ready to bring in a lysosome and have them fuse to destroy that bug. 01:03 And yet, you have diseases where you don't have that. 01:06 You don't have that fusion. 01:08 That's called Chediak-Higashi syndrome. 01:10 Again, a rarity, but it proves the point about the biological importance of each of these steps. 01:15 And these patients get recurrent infections. 01:18 And then you can have defects in microbicidal activity. 01:21 So there are patients who have defects in the NADPH oxidase, that's the one that's going to be responsible for getting protons into that primary granule, so that we can generate the oxygen free radicals and hydrogen peroxide. 01:35 And those patients get recurrent infections. 01:39 Gee. 01:41 Cleverly, some bacteria have learned how to make catalase. 01:44 They called it catalase is an enzyme that degrades hydrogen peroxide. 01:49 If the bacteria get into that primary granule, and it make a lot of catalase, we never make the hypochlorous acid. 01:55 We don't make the bleach, that's going to kill the bacteria. 01:58 And they do quite well. 01:59 So there are certain fairly nasty bugs that make catalase, and you will encounter those in microbiology. 02:07 And there's too much inflammation. 02:09 So again, a lot of the inflammatory mediators are pretty much nonspecific. 02:15 They will kill bacteria, pathogens, yes, but they will also kill normal tissue. 02:20 And you can have as you have here, ongoing inflammation that's just causing a lot of tissue necrosis and damage. 02:29 When you have nothing but pure neutrophils and bugs, that's abscess. 02:34 And there is no tissue left behind. It's just a collection of pus. 02:40 So that's exuberant, acute inflammation. 02:42 You can have a loss of function because of the appropriate acute inflammatory response. 02:46 So in pneumonia, we have bacteria in the lungs, we recruit neutrophils, we have increased vascular permeability, that's all part of getting rid of the bug and clearing the pneumonia. 02:57 But in the meantime, all the airspace is filled up with bacteria, and neutrophils, and water from the increased vascular permeability. 03:05 And so you may have diminished function. 03:07 You may have hypoxia. 03:08 That's just part and parcel of the normal response in the lung. 03:13 And then you can have a systemic effects of acute inflammation. 03:16 So, in sepsis, the appropriate response to elements of the bacterial cell wall will sometimes give a very profound cytokine activation. 03:27 When that happens, those cytokines that would normally in a localized environment just cause increased capillary, post capillary venial permeability, and will cause vasodilation. 03:41 Now, if you have those same mediators in the entire body, you have hypotension. 03:47 So in a localized environment, doing exactly the right thing, too much of the systemic mediators being released and you get no blood pressure, hypotension. 03:57 Normally too, in a localized environment, we will want to make the vessels procoagulant because we're anticipating there will be injury and we want them to clot appropriately. 04:07 And yet, if we do that now systemically because high levels of mediators, we will get thrombosis everywhere, not good. 04:16 So the combination of hypotension and systemic thrombosis, called disseminated intravascular coagulation is how septic shock manifests itself. 04:29 So you can have too little or too much. 04:32 Usually want to be right in the middle. 04:36 With that we've covered this huge range of territory having to do with acute inflammation. 04:41 The beginning of the process that will allow us to clear and digest dead stuff. 04:49 To get rid of the bacteria that may have caused the dead stuff, and then begin the process of healing.
About the Lecture
The lecture Defects in Acute Inflammation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Individuals with chronic granulomatous disease are susceptible to infections due to...?
- ...catalase-positive bacteria.
- ...encapsulated bacteria.
- ...enteroviruses.
- ...gram-negative bacteria.
- ...obligate intracellular bacteria.
Which of the following steps of leukocyte extravasation is affected in sialyl-Lewis X deficiency?
- Rolling
- Tight adhesion
- Diapedesis
- Migration
- Chemotaxis
Which of the following results from the disseminated activation of inflammatory mediators?
- Thrombosis
- Hypertension
- Abscess formation
- Gangrene
- Increased intravascular volume
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |