Playlist
Show Playlist
Hide Playlist
COVID-19 (SARS-CoV2) Pandemic: Timeline, Virology, and Vaccination
-
Slides Pandemics Epidemiology of COVID-19.pdf
-
Reference List Epidemiology and Biostatistics.pdf
-
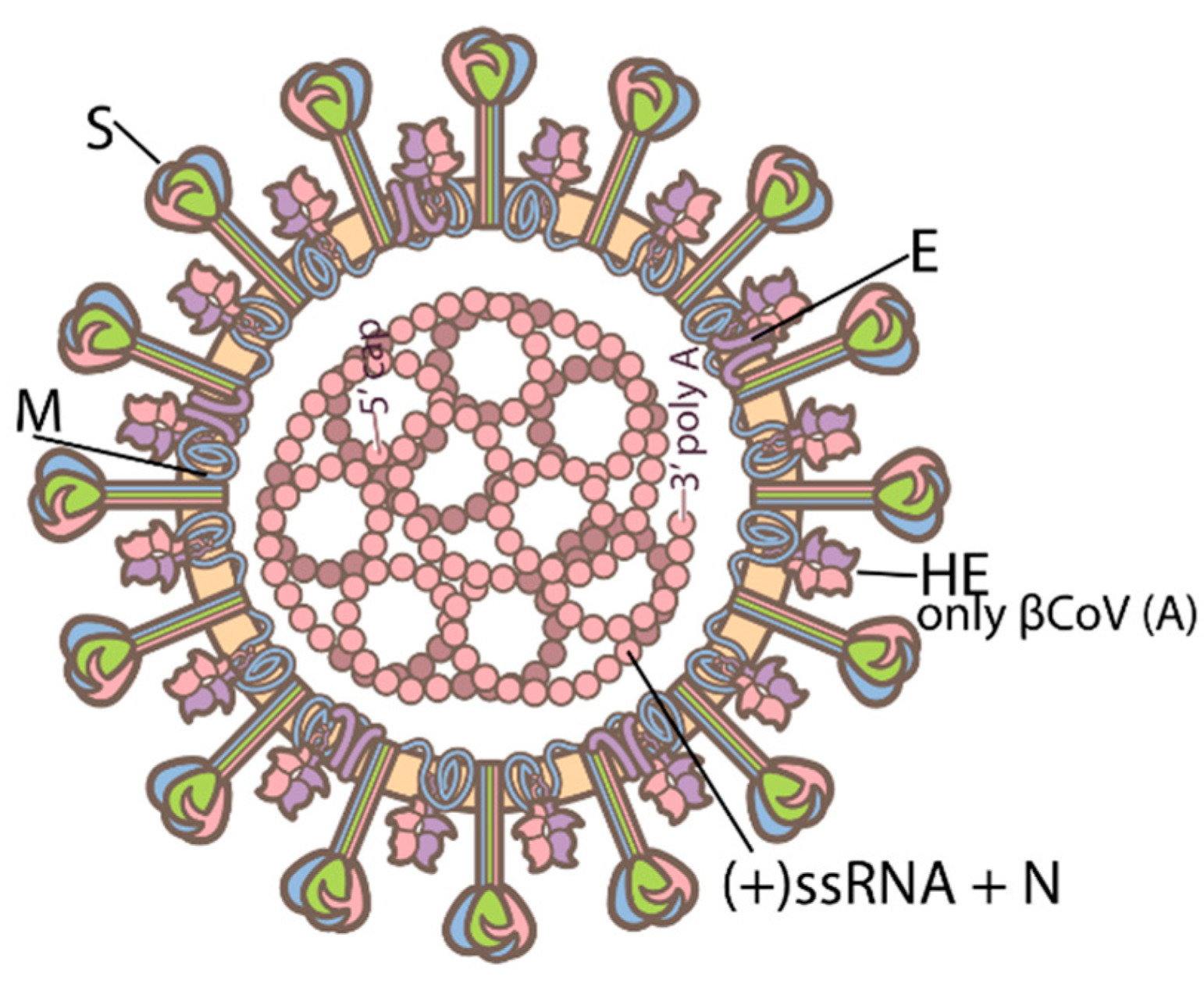
Download Lecture Overview
00:00 Hello, in this video we'll talk about COVID-19. 00:03 The epidemiology of COVID-19. 00:06 And how we think about it from a population health perspective? We'll talk about the timeline, the history of the disease, the virology of it. 00:14 We'll talk about the testing dynamic and the epidemiology of testing. 00:18 And lastly, we'll talk about, how we manage the disease? What are the challenges? And what can we do for population health perspective to help keep the world safe? Thank you. 00:30 Let's go over the timeline of the pandemic first. 00:34 In November of 2019, that's when we think the first official cases of this disease were detected in Hubei, China. 00:42 There is some controversy here. Some people claim that the disease may have been around earlier than that, but we don't know yet as of the recording of this video. 00:52 In December of 2019, in fact, the last day of the year, Chinese officials in Wuhan confirmed dozens of cases of a kind of pneumonia that some people were thinking was SARS, the return of SARS. 01:07 In January of 2020, the outbreak was indeed identified as a new coronavirus. 01:14 Very similar to SARS, called SARS-CoV-2. 01:19 Couple of days later, China reported its first known death from this new illness caused by this coronavirus. 01:28 And later on that month, the WHO confirms that the cases were detected outside of China. 01:34 At this point, people paying attention we're starting to get worried. 01:38 January 21st. 01:39 The USA announced its first confirmed coronavirus case. 01:44 Again, it may have arrived earlier but this is when it was first detected. 01:48 Two days later, Wuhan, a city of 11 million people was placed under quarantine, a city wide restriction lockdown. 01:58 In February, we have the first coronavirus death reported outside of China. 02:03 It was in the Philippines. 02:04 February 11th. 02:06 The disease finally had a name, COVID-19. 02:12 On February 24th, Italy officially becomes the epicenter of the epidemic. 02:20 When more cases and deaths were reported there than we had in China. 02:25 On March 10th. Italy now has locked down the entire country in an attempt to slow transmission. 02:32 March 11th. Finally, the World Health Organization declares COVID-19 to be a pandemic. 02:39 And in doing so, more resources are released and the entire organization swings into action to focus on this singular threat to global public health. 02:51 March 13th, the WHO declares Europe to be the new epicenter of the epidemic. 02:56 In March 16th, in Germany seals its borders. 03:00 March 18th, Canada and the USA close their shared border, the world's longest undefended border, now close to travel. 03:09 March 19th, China reports no new cases. 03:13 So, the first wave seems to be over in China. 03:16 March 19th. 03:18 Italy overtakes China as the worst-affected country in toto. 03:23 March 25th. The WHO warns the USA that they are likely to become the epicenter. 03:30 As most cases and are being detected in New York, a major travel hub and a crowded city, where transmission could be well achieved. 03:40 On June 2nd, over 6 million cases are confirmed with over 300,000 deaths in 188 countries. 03:48 And by October, we have 35 million cases and over a million deaths. 03:55 As of the recording of this video, January 1st, 2021, there are close to 85 million cases globally and close to 2 million deaths confirmed. 04:08 So, let's talk about the virus. 04:10 It is a single-strand RNA virus. Some viruses contain DNA. 04:15 This one contains RNA. 04:17 It's a type of coronavirus. 04:20 The name is taken from the spiky proteins on its surface that make it look like a crown or a corona. 04:28 In this sense, it's like a SARS or MERS before it or even the common cold. 04:34 We don't really know where it came from. 04:36 But we think might have originated in a bat. 04:39 And maybe it mutated in an amplifier species possibly a pangolin. 04:45 Possibly these two species interacted in the wet markets of Asia. 04:49 We don't really know. 04:52 We know that transmission occurs primarily via respiratory droplets from exhaling, talking, singing, coughing, and sneezing. 05:02 Now, we know that if you're simply exhaling, then the droplets tend to fall within a two meter range. 05:10 And if you're coughing or sneezing, you can propel them further. 05:13 We also know now that airborne or aerosol transmission is likely a viable route for this disease, which is a serious consideration because it means many indoor settings are not as safe as was earlier thought in the earlier months of the pandemic. 05:34 We know that peak viral load occurs about 4 to 5 days after infection. 05:41 And this is somewhat of an asymptomatic epidemic. 05:45 So, asymptomatic cases can be infectious. 05:49 And there's this incubation period of up to 14 days. 05:52 We have to distinguish here between asymptomatic and pre-symptomatic. 05:56 Asymptomatic individuals will never have symptoms. 06:00 Whereas, pre-symptomatic people will develop them. 06:04 But in both cases, it seems that individuals can transmit the disease without showing symptoms. 06:12 This is a controversial statement. 06:14 Some people claim that this is not a strong effect. 06:17 but the consensus is that it's a real thing. 06:20 And it's one of the characteristics of the epidemic that really confound our ability to control that well. 06:29 Now, the basic reproduction number is difficult to estimate. 06:32 But maybe it ranges from around 1 to almost 4. 06:37 We think that in China, it may have been up to 5.7. 06:40 Some people think is even higher than that. 06:42 Of course, it varies based upon the population dynamics of where it's being observed, population density, the behaviors of individuals, and so forth. 06:54 And some of the hardest hit long-term care centers in China saw very high reproduction numbers. 07:01 Indeed, the majority of deaths in the Western Hemisphere have been in long-term care centers. 07:09 That's where the elderly abide, and that's where they are more likely to be in close proximity with each other. 07:15 So, long-term care centers, nursing homes, were always going to be the places that we need to focus our control measures on and in many ways we failed them. 07:27 In recent months, a new variant has emerged. 07:32 This new variant is called by some B.1.17. 07:36 It was identified in the UK. 07:38 And it has some troubling characteristics. 07:42 We think that it has some mutations that allow it to be more transmissible. 07:49 This is likely due to the virus, being able to bind to the cell a bit better, and maybe being able to evade the immune system a bit better. 07:59 There are no signs yet that this new variant is more lethal, or can create different symptoms, or increase the probability of hospitalization once you're infected. 08:11 But it just seems to be transmitted more easily. 08:14 This is concerning from a population health perspective because even if the fraction of people who get sick, who then become hospitalized and or die, remains the same. 08:28 The fact that more people can now be infected means that the raw number of individuals becoming hospitalized and then die will increase, if this variant becomes the dominant variant. 08:40 So, efforts are underway to curtail international travel more so such that this variant does not find foothold in more countries. 08:54 Amazingly, several vaccines have been developed in record time, and they are being distributed around the world. 09:01 They embrace a variety of technologies, all of which rely upon the identification of the spike protein on the surface of the virus. 09:11 By protein is what allows the virus to bind to the cell. 09:15 It is the license plate, the identifying factor that allows the immune system to identify the virus. 09:25 Many approaches are being taken to develop vaccines. 09:28 Three have been shown to be quite effective. 09:31 The classical attenuated virus approach is being used by Sinopharm, for a Chinese manufactured virus. 09:40 So, a weakened version of the SARS-CoV2 virus is injected, and that causes an immune response. 09:48 Another technology is the viral vector approach. 09:52 This is the approach used by the Russian Sputnik V formulation and also the approach used by Oxford University and AstraZeneca, for their vaccine. 10:02 This is when another virus, a less problematic one. 10:06 In the case of the Oxford formulation, it's a chimpanzee adenovirus is genetically modified to have the SARS-CoV2 spike protein on it. 10:19 And so when a patient is exposed to this genetically modified adenovirus, they are infected, but don't become sick because this is a mild chimpanzee virus. 10:31 But the spike protein is introduced into their cells and their body produces antibodies against that spike protein. 10:39 Hence, they have neutralizing antibodies. 10:43 And lastly, the most scientifically new approach is the mRNA approach, messenger RNA approach, used by manufacturers Moderna, and Pfizer-BioNTech. 10:57 Essentially, this new approach injects messenger RNA into the patient and this messenger RNA interacts with Seiler ribosome to produce the spike protein. 11:12 Whereupon the body then creates neutralizing antibodies against this spike protein. 11:19 As of the recording of this video, at least three vaccines have been licensed for use in many countries and some countries have more than three. 11:30 So, we are witnessing an enormous global effort to have vaccine rollout.
About the Lecture
The lecture COVID-19 (SARS-CoV2) Pandemic: Timeline, Virology, and Vaccination by Raywat Deonandan, PhD is from the course Pandemics.
Included Quiz Questions
When does the viral load of SARS-Co-V-2 peak in a person who has contracted the disease?
- 4 to 5 days
- 2 to 3 days
- 6 to 8 days
- 12 to 15 days
- 9 to 11 days
When was the first case of COVID-19 reported?
- November 17, 2019
- December 16, 2019
- October 15, 2019
- September 17, 2019
- January 1, 2020
What is the nucleic acid structure of coronavirus?
- Single-stranded RNA virus
- Single-stranded DNA virus
- Double-stranded RNA virus
- Double-stranded DNA virus
- Multi-stranded RNA virus
What is the approximate Ro for COVID-19?
- 1.4 - 3.9
- 11 - 15
- 0.5 - 1
- 10 - 11
- 6.5 - 8.5
Which vaccine type is the newest technology to be used to create a COVID-19 vaccine?
- mRNA
- Viral vector
- Attenuated Virus
- Killed virus
- Antibodies
What protein of the B.1.1.7 variant is mutated?
- Spike protein
- Membrane protien
- Envelope protein
- Nucleocapsid protein
- Nonstructural protein
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |