Playlist
Show Playlist
Hide Playlist
Heart Failure (HF): Medications
-
Slides CongestiveHeartFailure CardiovascularPathology.pdf
-
Download Lecture Overview
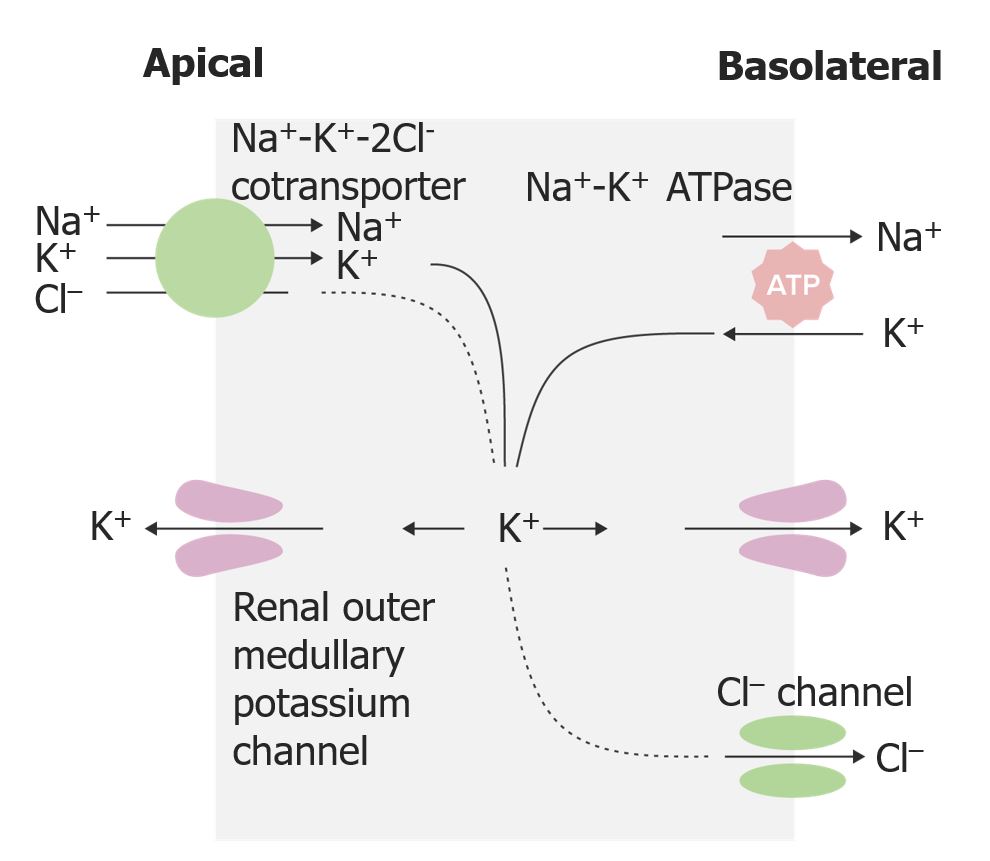
00:02 ACE inhibitors. Reduce SVR. What does that mean? Total peripheral resistance, systemic vascular resistance, how? You don’t have as much angiotensin II. Here we go. Reduces remodeling, ACE inhibitors first line of therapy with CHF because of the ability to reduce remodeling. 00:17 What does that mean? You do not introduce the repair process and cause further harm. 00:24 Do not start if your patient has acute renal failure. Is that understood? A lot of times remember your instances in which the kidneys require angiotensin II so that it can restore GFR or maintain GFR. So please make sure that you pay attention to renal status before you do give your ACE inhibitor. We have talked about this earlier when we did atherosclerosis with renal arterial stenosis as well. Keep that in mind. In addition, the side effect that you are looking for is a dry cough. In addition, you have the inability to properly metabolize what component with ACE inhibitor that results perhaps in cough? It is called bradykinin. What kind of effect that the bradykinin can have on your blood vessels? Increased vascular permeability. So what do I sound like? What does that mean? Angioedema. What is happening? The blood vessels around my oral mucosa undergo vasodilation, increase capillary permeability. And it is how I talk, you know that, which my impersonation of angioedema is. Will you forget this? Never. So ACE inhibitors, inability to properly handle bradykinin. Know that, for any exam, you will be in good shape. We talked about cough, angioedema, renal failure. What about this hyperkalemia? Important yeah. Remember, please. In addition, ACE inhibitor with angiotensin II and bradykinin, aldosterone does normally. What kind of effect does aldosterone normally have on potassium? It gets rid of it. If you have ACE inhibitor, they don't produce aldosterone from your glomerulosa. So, therefore, you are going to retain your potassium, hyperkalemia. Not good for whom? If hyperkalemia, EKG T tenting. Next, more importantly, what happens? The resting membrane potential and threshold. 02:25 So, the difference between those two, what happens now? Is that resting membrane potential going to become more positive or is it going to become more negative? You answer that question. 02:32 Way back in basics, everyone loves this question as you do. It is the fact that the resting membrane potential gets closer to threshold, it will depolarize. It gets closer. It is not a good thing. Very scary, especially for the heart. 02:46 ARBs. Angiotensin receptor blockers, pretty straight forward. Very analagous. If your patient is having dry cough and some of the intolerance of ACE inhibitor, then you will start thinking about using your losartan and such. Side effect. Hypotension, angioedema. You see dry cough is not here. 03:05 Recently, the angiotensin receptor-neprilysin inhibitor, sacubitril-valsartan, has been preferred over ACE inhibitor or ARB therapy. 03:14 In addition to the benefits of an angiotensin receptor blocker, sacubitril inhibits the degradation of peptides that promote vasodilation and natriuresis. 03:24 However, neprilysin inhibitors alone are not effective, as they also increase angiotensin II levels. 03:31 Thus, it is used in combination with an ARB to mitigate that effect. 03:36 This combination has been shown to improve mortality and reduce hospitalizations to a larger extent than ACE inhibitors or ARBs. 03:44 Beta-blockers. Metoprolol, carvedilol. You knock out the beta-1 receptors, should not be used in patients with CHF. It may blunt the tachy. Be careful and so, therefore, remember if you knock out the tachy, there might be a compensatory mechanism that needs to be taken place. So be careful. Side effects. Brady, heart block, hypotension, bronchospasms. Why? Especially be careful even when they say selective beta-1 blocker like metoprolol, you know is there such a thing as a guarantee? No right. So just because you say selective, yeah general scheme of things and definition, sure. However, is there a possibility that it might also have beta-2 blocking effects? Sure. What are you breathing in to relieve ashtma? Inhaler, beta-2 agonist. So there is every possibility that by giving a beta-blocker to a patient that has asthma you exacerbate the condition. 04:43 Please be careful. And that tachycardia is huge as well because there are times with the beta-blocker that might mask the events that might be taking place to who you win that your patient might be going into hypglycemia with diabetes. Keep that in mind. That is a huge pharmocologic point. So, once again, if you want to review some of you form, take a look at the conditions or what conditions would then exercise caution or great caution when using beta-blocker? For sure bronchospasms and diabetes mellitus are two big ones. Nitrates, We talked about this plenty. 05:22 It is the fact that here you have your longer acting causes vasodilation, both the venal and the arterial, decrease TPR and it also decreases your preload. In addition, used in combination with hydralazine in African Americans to decrease mortality. 05:44 Sodium-glucose cotransporter 2 (or SGLT2) inhibitors have also now been added to guideline-directed medical therapy. 05:52 There is much that we are still learning about this class of drugs, and many potential benefits in patients with heart failure. 05:58 These drugs are primarily known for their effects on the kidneys, where they reduce renal tubular glucose reabsorption. 06:05 This promotes diuresis and natriuresis, which reduces preload. 06:09 In addition, they appear to improve endothelial function and vasodilation, which can improve blood pressure and reduce afterload. 06:16 There is also a belief that these medications may work through multiple mechanisms to improve energy metabolism and decrease oxidative stress on the heart. 06:24 While they were originally used in the management of diabetes, patients without diabetes also benefit from these cardiovascular effects. Side effects to be aware of include an increased risk of genitourinary infections and volume depletion (which can lead to acute kidney injury). 06:41 Additionally, diabetic ketoacidosis (even with normoglycemic levels) has been seen in patients with type 1 or 2 diabetes. 06:51 Spirinolactone, what do we do in here? Here is your class III and IV heart failure. What does that mean? Minimal exertion. Oh no, I am having symptoms for even symptoms at rest. "Hey doc, I can't even sleep on my bed. I can't even sleep in a supine position." Well I am not going to tell you that but I have to go sleep where? On my recliner chair. Sad. III and IV indicated spirinolactone. If you knock out your aldosterone, you have hyperkalemia. 07:19 Hence, it is called potassium sparing drug and not only that but spirinolactone has what kind of effect? It is the other hormone that it can also antagonize. Please tell me what that hormone is. An androgen antagonist, isn't it? Where does that come in handy? Something like polycystic ovarian syndrome. Here is a patient with polycystic ovarian syndrome. She is a female, genotypiclly XX. She walks in, but she has hirsutism, male-like hair features. So there's a lot androgens in that patient, polycystic ovarian syndrome and that is clinically true because you are actually looking for LH being greater than FSH. You are with me here? If you don't, that is okay. That is quite right because you will come in to spirinolactone. Later on we will talk about polycystic ovarian syndrome and how you want to manage that? With there, we will talk about spirinoloactone because it is an androgen antagonist. But in the process may give you gynecomastia. 08:15 There is something called ICD. You want to make sure that you at least know what it stands for. Implantable Cardioverter Defibrillator. Nowadays you know that it is pretty much found in everywhere. Thank goodnes. Advanced heart failure because you are worried about that arrhythmia. And well with these hopefully you will be able to prevent from arrhythmia kicking in. We talked about what arrhythmia means. It just means that once you disrupt the architecture of the heart, then you are prone to whatever type of arrhythmia it may be. Now a couple of things here. Post MI 40 days, implantable or nonimplantable with ejection fraction less than 35? And here once again class II and III, which means that you have moderate exertion with symptoms and minimal exertion. Please make sure you go back to take a look at your New York Heart Association classes so that you are familiar with the symptoms of your patient. 09:06 Side effects. Expenses obviously quite complications, not all will benefit. And inappropriate shocks which you might be feeling with a defibrillator which your patient might then be complaining of.
About the Lecture
The lecture Heart Failure (HF): Medications by Carlo Raj, MD is from the course Heart Failure: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT a potential side effect of beta blocker therapy in CHF patients?
- Tall T waves on ECG
- Suppression of tachycardia in hypoglycemic diabetic patients
- Bronchospasm
- Heart block
- Hypotension
In a patient taking lisinopril, which of the following side effects may be alleviated by switching to losartan?
- Dry cough
- Dizziness
- Hyperkalemia
- Hypotension
- T-tenting on ECG
ACE inhibitors are used as first-line therapy for congestive heart failure patients. Which of the following is NOT a contraindication for ACE inhibitor therapy?
- Diabetes
- Acute renal failure
- History of angioedema
- Renal artery stenosis
- Hypertrophic obstructive cardiomyopathy
Which of the following medications is associated with gynecomastia?
- Spironolactone
- Metoprolol
- Lisinopril
- Isosorbide mononitrate
- Losartan
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
Great content, the useful facts are well explained! Dr Raj is a great professor.
would be much more useful if he didn't rush and actually explained the mechanism of action. I'm much better off reading a textbook than watching this