Playlist
Show Playlist
Hide Playlist
Complement System & Chronic Inflammation – Inflammation and Wound Repair
-
Slides Inflamation Cellular Pathology.pdf
-
Download Lecture Overview
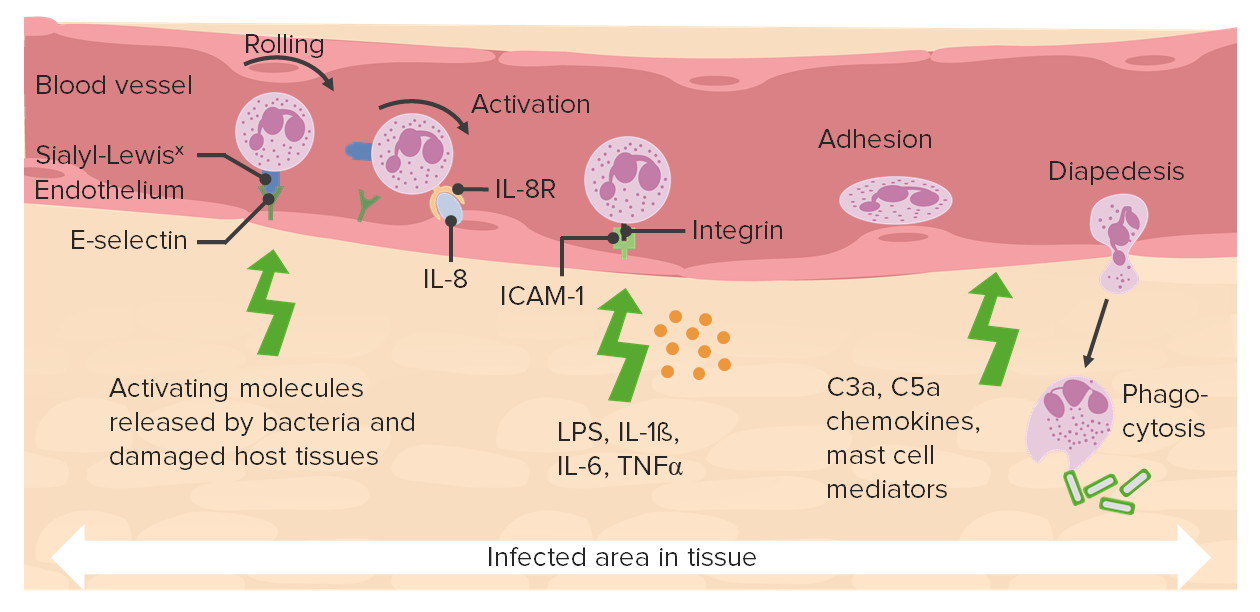
00:01 The complement system and how it relates to what we talked about with inflammation. Remember when I talked to you about a silly little story called strawberry and chocolate. This is opsonin. So C3b is going to opsonize the bacteria making it mighty tasty for whom? The neutrophil. Then you have anaphylatoxin C3a. C5a remember is a chemotactic factor. 00:28 What does that mean? Once neutrophil comes out in interstitium, this is the GPS. It will tell the neutrophil where to go. 00:37 And the MAC complex, membrane attack complex, C5 to C9 will be responsible for then boring a hole through the bacteria in which through osmotic pressure all the fluid accumulates within the bacteria and it perishes. Important complement. 00:55 In complement pathologies, we'll talk about over and over again including hereditary angioedema. Meaning to say that now you've lost you C1 inhibitor. Too much complement activation resulting in oedema in the oral mucosa, inflammation, difficulty talking. Other complement pathologies that we have dealt with include paroxysmal nocturnal hemoglobinuria with the deficiency of DAF and MIIL. That's CD55 and 59 respectively. Other complement pathologies that you dealt with in microbiology. 01:32 If you are deficient of MAC you are now susceptible to Neisseria species. And another important complement pathology known as your MPGN type II in which you have a nephritic factor which then stabilizes my C3 convertase. All of this we've talked about and all i'm doing is just reinforcing them. And at this point, with a review, you're thinking, Oh yeah I know this. 01:58 Good. Let's continue. Cytokines involved with mediators of inflammation. We talked about interleukin-1 and TNF a part of your rolling system. Acute phase reactant. Interleukin-6 plays a pretty big role with fever along with interleukin-1. 02:19 Interleukin-6, we have also looked at with what's known as your anemia of chronic disease. Also cytokines here release neutrophil from bone marrow. And you need certain interleukin that are responsible for this. Including interleukin-17. 02:36 Nitric oxide is a major vasodilator and also a type of free radical. It's bactiricidal. Nitric oxide. Remember you want to do everything in your power in acute inflammation to vasodilate. Chronic inflammation is where we move on next. 02:58 With chronic inflammation, well now let's say that give me an example here. If it's acute myocardial infarction. 03:05 Acute myocardial infarction let's say within the first day, neutrophils come in. Three days later, the neutrophils undergo apoptosis and it's being replaced by this cells. We have lymphocytes and take a look at the specific lymphocyte that is blown up for you. The nucleus of a lymphocyte should be approximately the size of your RBC's but here specifically were in our tissue. Okay. So, lymphocytes and macrophages will play huge roles and lymphocytes will then be responsible for well, B-cell will differentiate into a plasma cell. Take a look at that plasma cell and then within your cell you find rows and rows of rough endoplasmic reticulum. Because you need this for proper immunoglobulin production. Chronic inflammation, the key cells include macrophages, lymphocytes and B-cell abviously is going to differentiate into a plasma cell. Examples here, necrosis with chronic inflammation. Fibrosis is going to be more of an issue. Granulation tissue and immunoglobulin G, IgG. 04:18 So the necrosis at this point is more or less contained and it's more about the repair process. Meaning to say that you are trying to contain your inflammation. Maybe perhaps a granuloma is necessary to inprison my foreign body. Maybe TB. 04:36 Maybe granulation tissue is required for proper wound healing which we will talk about upcoming. And if you are dealing with chronic inflammation the immunoglobulin that you are referring to always will be IgG in chronic inflammation. With chronic inflammation, a granuloma. What must you have within a granuloma in which you would then imprison my let's say a bacteria such as tuberculosis. 05:09 Well you must have an epitheloid cell. An epitheloid cell would be fused macrophages. And by definition you should have at least three epitheloid cell which is then creating granuloma. Do not get your granuloma confused with a granulation tissue. 05:27 Think about the different places where you can have a granuloma. With a TB infection, that will be a caseous but nowadays in Pathology we call this an infectious type of granuloma. And this granuloma could be located in the lungs, but very well could be located in other organs including your heart, including the liver, including the bladder. Or it could be non-caseous such as sarcoidosis, such as berryliosis, such as Crohn's disease. All this would then have a granuloma but that would be non-caseous type. Remember that this for the most part tends to be a type IV hypersensitivity. And the surrounding cells that you would find off a granuloma would in fact be CD4 cells. And CD4 cells specifically it's helper T 1 type in which it's responsible for conducting or creation or maintanence of a granuloma. One thing that you want to worry about unfortunately, is that now as you become more advanced with our pharmacopeia that you have drugs that are called TNF inhibitors including infliximab. Infliximab is a major TNF inhibitor in which when it's used let's say for example autoimmune diseases such as your such as your rheumatoid arthritis. And if your patient had a TB infection, you're worried about reactivation. Reactivation of the TB.
About the Lecture
The lecture Complement System & Chronic Inflammation – Inflammation and Wound Repair by Carlo Raj, MD is from the course Cellular Pathology: Basic Principles with Carlo Raj.
Included Quiz Questions
A deficiency of a component of the membrane attack complex (MAC, C5–C9) is associated with infection by what type of organisms?
- Neisseria species
- Chlamydia species
- Streptococcus species
- Staphylococcus species
- Haemophilus influenza b
Which of the following is a very potent vasodilator?
- Nitric oxide (NO)
- Interleukin-6 (IL-6)
- Interleukin-17 (IL17)
- MAP Kinase
- Interleukin-1 (IL-1)
Which of the following is NOT a characteristic of chronic inflammation?
- Increased necrosis
- Increased IgG
- Fibrosis
- Increased granulation tissue
- Increased number of plasma cells
Which of the following are required for the production of granulomas?
- TNF
- IL6
- NO
- C5a
- IgG
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr Raj is so good at reminding associated pathologies!!! Perfect for an overview