Playlist
Show Playlist
Hide Playlist
Colorectal Cancer Staging with Case
-
Slides Large Intestine.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
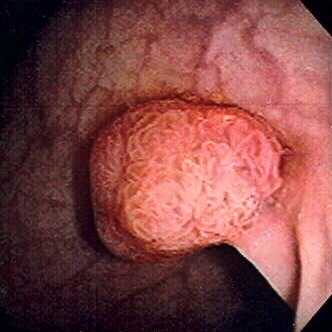
00:01 We'll move on to our next case. 00:04 A 39-year-old woman presents to the clinic complaining of bloody stools for one week. 00:09 She has a history of ulcerative colitis, diagnosed at age 29, well-controlled on a combination of corticosteroids for flares and mesalamine. 00:19 Her last flare was several years ago. 00:21 She has not had abdominal pain, fevers, diarrhea or other changes in bowel habits. 00:26 She does note an 8-kg unintentional weight loss over the last 6 months. 00:31 Her vitals are normal, physical exam is unremarkable. 00:34 Her labs show a hemoglobin of 9 with an MCV of 78. 00:40 Her leukocyte count and sedimentation rate are normal. 00:44 What is the best next step in diagnosis? So let's look at some key features here. 00:51 She had new-onset hematochezia, with a known history of ulcerative colitis. 00:58 She currently does not have any features of a UC flare, but her weight loss is a bit concerning. 01:05 And on her labs, she has a microcytic anemia which can hint at long-standing blood loss. 01:14 In addition, her other labs, her white count and her ESR are actually reassuring against an ulcerative colitis flare, at present. 01:24 So, as a quick aside, know that whenever a patient describes a change in their bowel habits, new-onset blood in their stools or hematochezia or melena, and iron deficiency anemia, you should always consider colorectal caner. 01:41 This is a "must not miss" diagnosis and so you should always make sure to screen for and rule this out. 01:49 So let's talk a bit more about colorectal cancer. 01:52 Most colorectal cancers are adenocarcinomas. 01:57 Patient's presentation can vary quite a bit. 02:00 They may be asymptomatic and just havecancer detected on a routine screening, They may be symptomatic with GI bleeding, abdominal pain. 02:09 you might first catch them with iron deficiency anemia. 02:13 They may have change in their bowel habits, or they may have unintentional wight loss. 02:17 Rarely, they may present as an emergency with colonic obstruction or perforation leading to peritonitis. 02:26 So the diagnosis is usually made by colonoscopy as this is the most sensitive and accurate method for making the diagnosis. 02:35 And treatment as with all cancers, depends on the staging. 02:41 When this is a limited stage cancer, you can often do surgical resection. 02:45 but those who have more advanced cancers may undergo chemotherapy with 5-fluorouracil or radiation. 02:53 There are also newer molecularly targeted therapies that can target specific molecules in an individual's cancer. 03:00 These include immune checkpoint inhibitors like nivolumab or ipilimumab, which can be used for patients whose cancer has high levels of microsatellite instability. 03:10 In addition, patients often undergo post-treatment surveillance with colonoscopies and CT of the chest abdomen and pelvis at frequent intervals. 03:21 So we spoke a little bit broadly about the staging of colorectal caner. 03:26 Here you can see that in stages 1,2,3 - the cancer has slowly progressed to the layers of the mucosa, submucosa and eventually into the muscle. 03:36 Once it has reached the serosa or the outer layer of the colon wall and penetrated into the other organs or outside of the colon, you now have stage 4 cancer. 03:49 So, what other inherited or existing conditions can make somebody more likely to develop colorectal cancer? We spoke earlier about some broad risk factors that place the general population at risk for colorectal cancer. 04:04 But there are also very many familial cancer syndromes that can lead to very elevated risk of cancer. 04:11 We're not gonna go into too much detail here but these are some the syndromes you should know about for test-taking purposes. 04:18 So the first is Lynch syndrome or Hereditary Non-polyposis Colon Cancer. 04:23 This is from a mutation in a mismatch repair gene gene that can lead to many types of cancers listed here. 04:29 Patients may also have FAP or familial adenomatuos polyposis This is from a mutation in the APC tumor suppressor which leads to many adenomas forming throughout the GI tract. 04:42 You may also encounter Peutz-Jager Syndrome which is a mutation in the STK11 tumor suppressor which leads to the formation of many hamartomas throughout the GI tract. 04:53 Another type of syndrome is Juvenile Polyposis Syndrome which is a mutation in the TGF-beta signaling pathway again leading to hamartomas throughout the GI tract. 05:04 And lastly, an important one to know about is ulcerative colitis or Crohn's disease, so when patients have long-standing colitis and inflammation that occurs over and over, this places them at high-risk for colorectal cancer as well. 05:21 So, how often should individuals with any of these syndromes be screened for colorectal caner? This is a complicated answer and I will include the slide here for your reference. 05:33 What I would just draw your attention to, however, is that ulcerative colitis and Crohn's colitis patients with these conditions should be screened about every 1 to 2 years with a colonoscopy. 05:44 starting 8-10 years after they were first diagnosed with IBD So now that we've gone through that, let's go back to our case. 05:55 We have a 39-year-old woman with new-onset hematochezia. 05:59 She has a known history of ulcerative colitis. 06:02 She was diagnosed 10 years ago at age 29. 06:05 She currently has no features of a UC flare and her labs are mostly reassuring against this. 06:11 However she does now have a new-onset microcytic anemia which could be an iron-deficiency anemia from long-standing blood loss. 06:19 So the next best step in diagnosis is a colonoscopy to evaluate for a colorectal cancer, Thank you very much for your attention.
About the Lecture
The lecture Colorectal Cancer Staging with Case by Kelley Chuang, MD is from the course Disorders of the Small and Large Intestines.
Included Quiz Questions
Which of the following is the colonoscopy screening interval for patients with ulcerative colitis or Crohn colitis?
- Every 1–2 years, starting 8–10 years after diagnosis
- Every 2–3 years, starting at age 15 years
- Every 2–3 years, starting at age 18 years
- Every 1–2 years, starting at age 20–25 years
- Every 2–3 years, starting at age 25–30 years
Which of the following is the most accurate diagnostic test for colon cancer?
- Colonoscopy
- Abdominal CT
- Abdominal X-ray
- Sigmoidoscopy
- Abdominal ultrasonography
Which of the following mutations results in Lynch syndrome?
- Mutation in mismatch repair genes
- Mutation in APC tumor suppressor
- Mutation in STK11 tumor suppressor
- Mutation in the TGF-beta signaling pathway
- Mutation in the RB1 tumor suppressor
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |