Playlist
Show Playlist
Hide Playlist
Colon Cancer: Risk Factors, Diagnosis & Treatment
-
Slides Small and large bowel.pdf
-
Download Lecture Overview
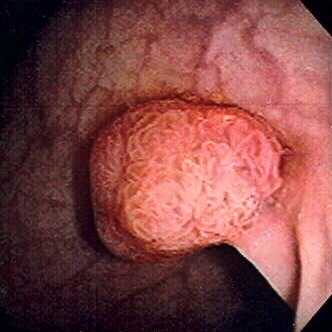
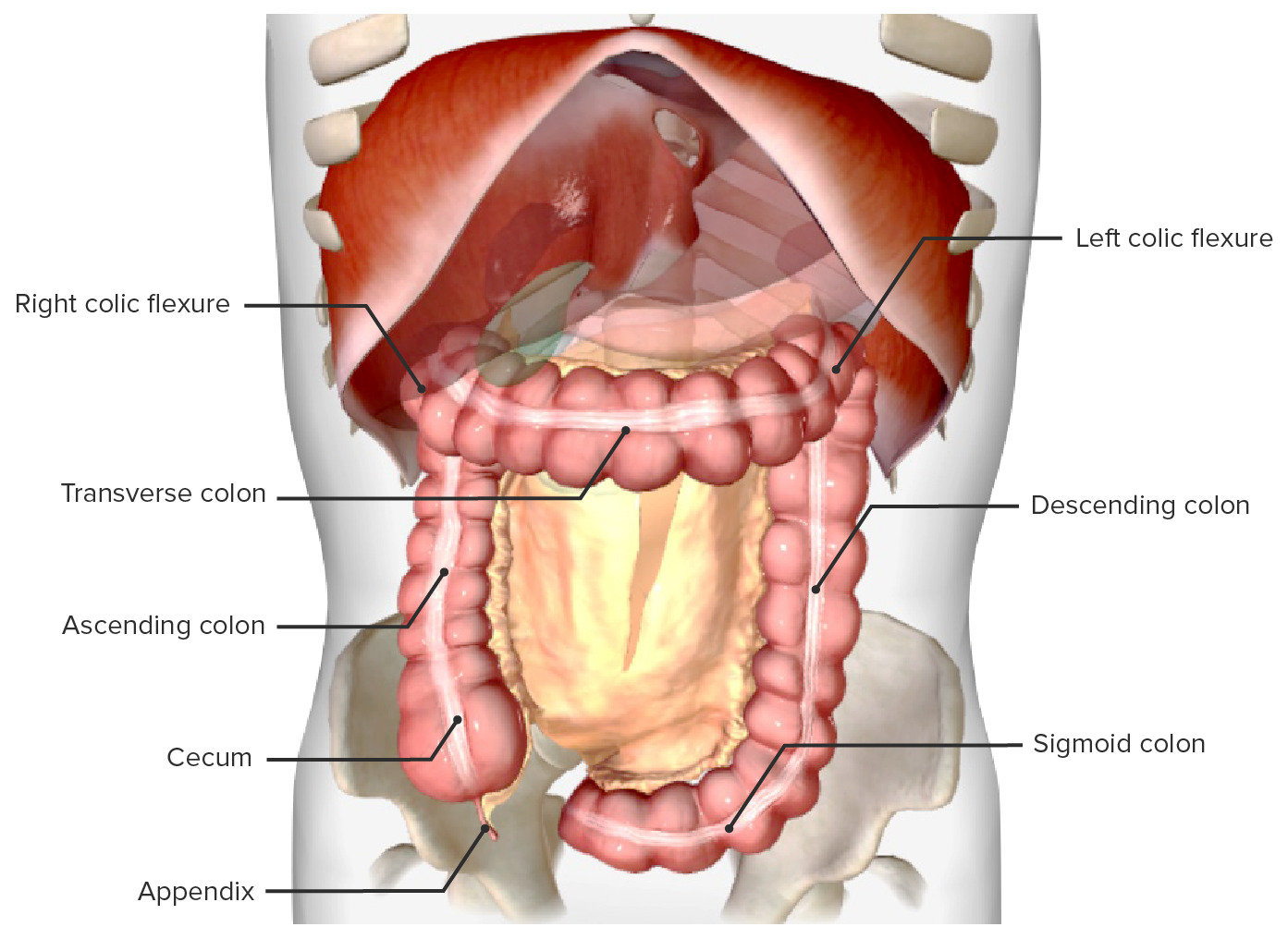
00:01 Our topic now is colon cancer. 00:03 It's the fourth most common cause of cancer in the United States. 00:06 And the second most common cause of cancer death. 00:09 Dr. Raj, I thought this was a number three. 00:12 Yeah, it is. 00:13 What do you mean? How could we both? Listen, if you were to separate the genders and the sexes, males and females. 00:22 Mortality. 00:23 Males: Number one, lung cancer; number two, prostate; number three, colorectal cancer. 00:31 Females. Mortality. Number one, lung cancer. 00:37 Number two, breast cancer. Number three colorectal cancer. 00:42 So, you just don't use third, correct? But if you combine your genders... Oh... 00:50 When combined for both genders, it becomes the second most common cause of cancer death. 00:54 That's up there. 00:56 Age: greater than 40. 01:01 Low fiber, high fat diet. 01:05 Personal history of colonic adenoma or cancer. 01:10 History is big. 01:11 Long-standing. 01:15 Such as inflammatory bowel disease, especially ulcerative colitis. 01:20 No joke. 01:22 Family history: Sporadic colon cancer, and HNPCC. 01:27 Hereditary nonpolyposis colorectal cancer Nonpolyposis. 01:34 Now, pause here for a second. 01:37 I want to bring two things to light here so that we're clear moving forward. 01:43 HNPCC. Remember that colorectal cancer What do you want to do? You want to divide this into really two types. 01:49 Just like we did for primary gastric adenocarcinoma. 01:52 We talked about two types there. 01:55 You have two types here. 01:56 But two types here. 01:58 literally, anatomically, location wise. 02:01 You have left sided, right sided. 02:04 Left sided, descending colon; right sided, ascending colon. 02:10 Genetically, amazingly, pay attention. 02:14 HNPCC. Hereditary Nonpolyposis Colorectal Cancer. 02:19 Remember biochemistry, microsatellite instability. 02:22 You've heard of MLH and MSH and such. 02:26 That will give rise to much more, so, right side of colorectal cancer. 02:30 Memorize that. 02:32 Whereas, if it's Familial adenomatous polyposis then it'll be left side of colorectal cancer. 02:38 What do you know about FAP? 100% of going on to colorectal cancer. 02:42 No joke. No, the genetics here big time. 02:48 Diagnosis: Slow growing tumor may present as iron deficiency, especially if it's right sided. 02:56 Could you find blood with left sided? Remember, you've heard a napkin ring or circumferential? So you have a ring around a napkin squeezing the napkin, "the napkin is the colon." Left sided, the descending colon. 03:11 You're squeezing strangulating it. Is that clear? That's left sided. 03:14 So the circumferential pattern, and napkin ring is the left side, apple core. 03:20 Once again. Could you find beating there? Sure, but that's more altered bowel habit. 03:26 On the right side, we'll talk about the description it's called polypoid. 03:31 And with the polypoid, much more so involved with bleeding and iron deficiency. 03:38 Abdominal pain, change in bowel habits much more so with left sided. 03:43 Perforation is a complication we're worried about, and rectal bleeding obviously will be taking place with both. 03:49 But much more so with right, and therefore iron deficiency. 03:55 Your tests for diagnosis include colonoscopy is the test of choice here. 04:00 Remember the colonoscopy, you want to use prudently. 04:03 And a patient that made them present with diverticular disease acutely. 04:07 But in colorectal cancer, my goodness, it is detested choice. 04:11 And your tumor marker, not sensitive, but prognostic evaluation is important known as CEA. 04:18 Carcinoembryonic antigen. 04:21 And of course, some of the new things that you want to pay attention colorectal cancer include your KRAS. 04:28 And with management, remember, not only would you have drugs such as your Leucovorin and company, but then you have a drug cost cetuximab which is then addressing your receptor tyrosine kinase. 04:39 Those are molecular pharmacology that you want to be familiar with. 04:44 Let's talk about colonoscopy in colon cancer, test of choice. 04:49 With the colonoscopy very rarely would ever ask you anything about sigmoidoscopy? Because if you were to only do and examine or investigate the sigmoid, what if you had a cancer on the right side? What if you had a polyp on the right side? You would miss it completely. 05:03 And hat makes no sense. 05:04 We know for a fact that a second leading killer overall third, leading killer individually engenders. 05:13 So, therefore, never choose sigmoidoscopy, when you're dealing with a colonoscopy. 05:16 You do a full colonoscopy to make sure that you catch anything on the right side. 05:22 This particular lower colonoscopy is showing you decreased caliber of the lumen of your colon. 05:31 And you see a little bit of blood as well. 05:33 You notice here, but this colonoscopy that you would have altered bowel habits as you're coming down the descending limb. 05:42 The left side we show you what's known as circumferential. 05:45 The left side oftentimes referred to as being, apple core. 05:49 And you might have heard this being used as napkin ring. 05:55 Colon cancer prognosis, it's important that you pay attention to staging. 05:59 On a boards, nowadays, whatever board that you're taking, I understand the staging becomes important because it tells you, well, prognosis goes from relatively maybe decent, to absolutely poor. 06:12 The staging system for colon cancer is known as the SEER system. 06:15 And it's based on three categories. 06:18 Localized: where there's no sign of spread outside the colon or rectum. 06:21 Regional: where the cancer has spread to nearby tissues or structures. 06:25 Or distant: Where the cancer spread to distant parts of the body such as the liver or lungs. 06:30 And their survival rates are 91%, 72%, and 14%. 06:36 Once you get the D, you're gone. 06:38 What that means is that metastasis taking place, and with colorectal cancer, you can either choose hematogenous or lymphatic spread. 06:47 And if it chooses hematogenous spread therefore, the number one place that metastasized to colon to the liver. 06:55 Alright? Colon to the liver. 06:58 From the liver, then maybe perhaps up into the lungs. 07:02 Management: surgery with wide resection, adjuvant chemotherapy, radiation therapy, especially when you start getting into Duke staging... 07:10 B B B as in boy. 07:14 Prevention: screening, screening, screening. 07:17 Age 50 years of age, a general population. 07:19 Keep in mind because of low fiber, high fat diet type of issue. 07:23 Age 40 years, 10 years, prior to diagnosis, if you're thinking about a patient, and the relative is in fact affected 10 years younger. 07:32 So, kind of behaves like you're mammography and a female with breast cancer, doesn't it? Beginning eight years if you're thinking about a patient with the inflammatory bowel disease of the ulcerative colitis type Prevention: Test for screening, colonoscopy. 07:51 A cold blood testing, and virtual colonoscopy. 07:54 Nowadays, of course, is playing a major role.
About the Lecture
The lecture Colon Cancer: Risk Factors, Diagnosis & Treatment by Carlo Raj, MD is from the course Small and Large Intestine Diseases: Basic Principles with Carlo Raj. It contains the following chapters:
- Colon Cancer - Clinical Presentation
- Colon Cancer - Diagnosis
- Colon Cancer - Prognosis, Treatment & Prevention
Included Quiz Questions
In what order would you place cancers according to mortality in the US, starting with the MOST common cancers?
- Men — Lung cancer, prostate cancer, colon cancer Women — Lung cancer, breast cancer, colon cancer
- Men — Colon cancer, prostate cancer, lung cancer Women — Colon cancer, breast cancer, lung cancer
- Men — Prostate cancer, colon cancer, lung cancer Women — Breast cancer, colon cancer, lung cancer
- Men — Lung cancer, prostate cancer, gastric cancer Women — Lung cancer, breast cancer, cervical cancer
- Men — Lung cancer, gastric cancer, prostate cancer Women — Lung cancer, cervical cancer, breast cancer
Which of the following is NOT a common risk factor for colorectal cancer?
- High-fiber diet
- Low-fiber diet
- Long-standing inflammatory bowel disease
- Hereditary polyposis syndrome
- Colorectal adenoma
A 65-year-old patient presents with iron-deficiency anemia. The fecal occult blood test shows positive results. Which of the following is the investigation of choice to perform?
- Colonoscopy
- Proctoscopy
- Ultrasound
- X-ray of the abdomen
- Sigmoidoscopy
What tumor marker is associated with prognostic significance in colorectal cancer?
- CEA
- Inhibin
- Beta HCG
- CA 19-9
- CA 125
Which oncogene is tested for mutational status in colorectal carcinoma and has therapeutic implications?
- K-ras
- RET
- Src
- Wnt
- Myc
What is the MOST common organ involved in distant metastasis of colorectal carcinoma?
- Liver
- Bone marrow
- Breast
- Brain
- Spleen
According to SEER staging, which of the following best describes the stage of a patient with colorectal cancer and a 5-year survival rate of 72%?
- Regional lymph node involvement
- Involvement limited to the submucosa
- Involvement beyond the submucosa without lymph node involvement
- Distant metastasis to liver
- Distant metastasis to the brain
Which of the following statements regarding screening for colon cancer is FALSE?
- In FAP disease, screening starts after 50 years of age.
- Screening starts when people are 50 years old.
- Screening is by colonoscopy.
- Screening in a patient who has a first-degree relative with the disease is at 40 years (or 10 years before the first-degree relative was diagnosed).
- Screening must begin after 8 years of inflammatory bowel disease of the colon.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |