Playlist
Show Playlist
Hide Playlist
Cholinomimetic Activators and Effects
-
Slides Cholinomimetic Activators Effects.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
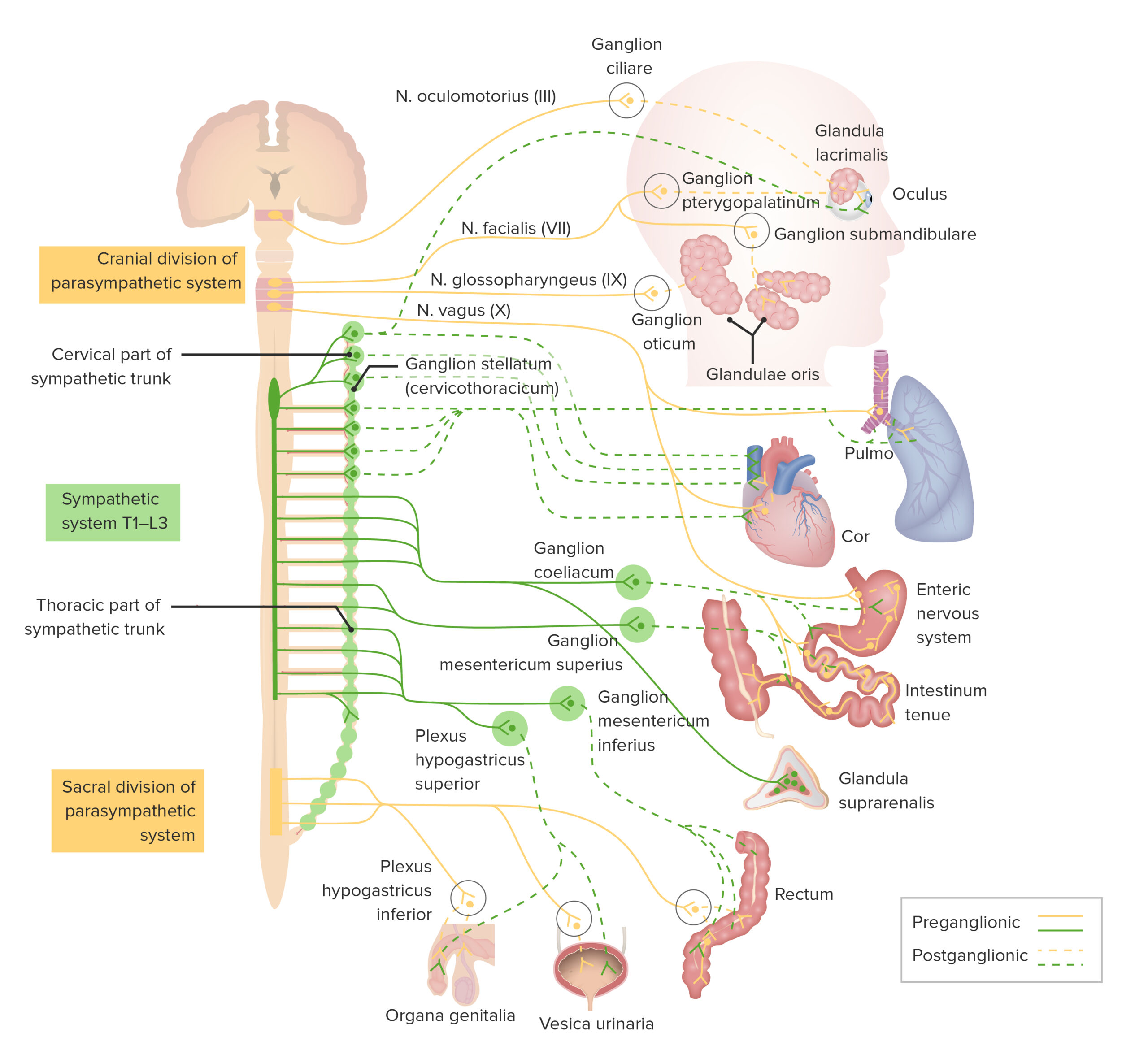
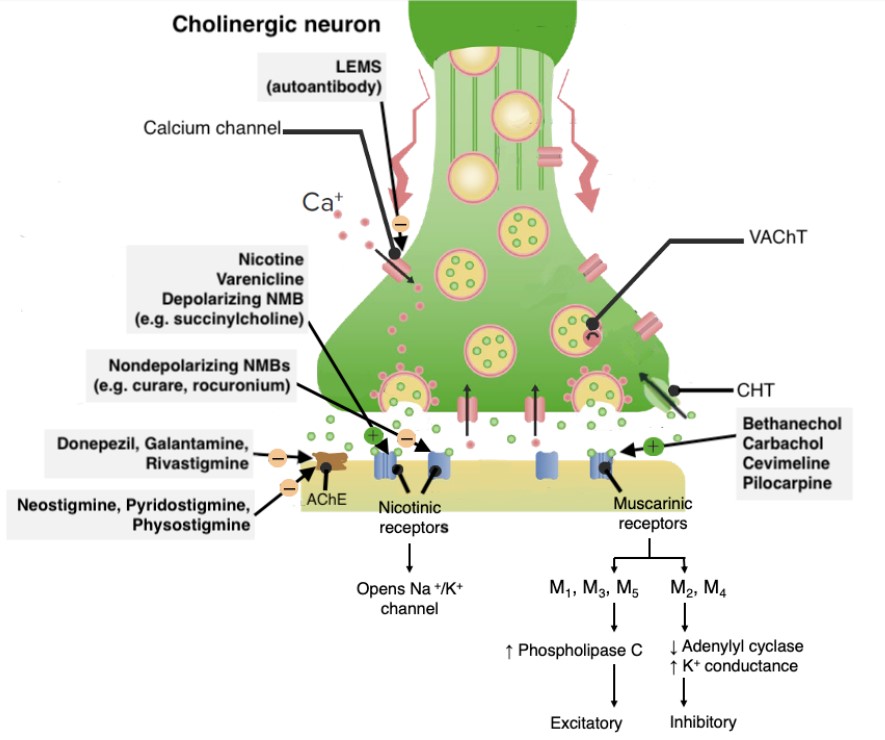
00:00 Hi. I'm Dr. PJ Shukle, we're going to continue the discussions about the pharmacology of the autonomic nervous system. Now we have many different types of cholinomimetics that act as direct activators. There are those that act on the muscarinic cholinergic receptors and those that act on the nicotinic cholinergic receptors. 00:23 So there are esters of choline like acetylcholine and carbacol that act on both, while methacoline and bethenicol only act on the muscarinic cholinergic receptors. 00:34 We also have some alkaloids that can work on the muscarinic cholinergic receptors, including pylocarpine. 00:41 Choline and lobeline are alkaloids that act chiefly on the nicotinic receptors. 00:46 Now let's take a quick look at the synaptic cleft in the autonomic nervous system. So specifically this is a cholinergic synaptic cleft and you can see that there is acetylcholine that is being released by the vesicle into the synaptic cleft. 01:02 So you see ACH there, that's acetylcholine. It would normally interact with a cholinoreceptor. 01:09 Now, if that acetylcholine is in the synaptic cleft for too long, it will get broken down by acetylcholinesterase or ACHE into choline and acetate. If we block acetylcholinesterase, we increase the levels of acetylcholine in the synaptic cleft and you have more excitation of the cholinoreceptors. We can have indirect activators of the system through this acetylcholinesterase inhibitor. Edrophonium is a good example of a short-acting agent that lasts between 5 and 15 minutes. Intermediate-acting agents can include neostigmine and physostigmine and this is often used in the treatment of myasthenia gravis and long-acting agents are often thought of as poisons or toxins and we see that with a lot of organophosphate such as malathion, parathion, and others that are used as pesticides. Now there is another long-acting agent that I just want to quickly mention. Sarin was used in the 1995 Tokyo attacks and it had devastating effects. So let's go to 1995 in Tokyo. What happened was was that this organophosphate was released into a subway system and patients ended up having death within minutes. They developed asphyxia. There is significant persistent neurological damage in those survivors. Now, why did some of these patients leave? Because there is some particularly astute doctors who are working in the emergency departments nearby the subway stations that immediately recognized what was going on, not because they had ever experienced this particular toxin or terrorist agent before but because they recognize the neurological symptoms of acetylcholinesterase and so they knew that the antidote to this would be atropine. 03:07 The physicians knew that the antidote to the cholinergic symptoms would be atropine, which blocks muscarinic receptors to counteract cholinergic overstimulation. 03:17 However, after seeing the severity of the symptoms, they added pralidoxime (2-PAM) to reactivate the acetylcholinesterase enzyme by cleaving the organophosphate-enzyme bond before it became irreversibly aged. 03:31 in the event of this kind of terrorist attack. So what was it that these astute emergency room physicians noticed about their patients? Well, they knew that these syndromes that these patients were experiencing were very similar to exposures, toxic exposures to some of the organophosphate pesticides like malathion and parathion. They also noticed that they had physiological effects similar to the administration of medicines like pyridostigmine, neostigmine, or physostigmine. And what were those clinical findings? Well, in the eye they notice that patients had a contraction of the circular or sphincter muscle of the iris. This causes pupillary contraction or what we call myosis. This is used in near vision accommodation so this is why they were able to tell just by looking at the pupils that these patients had been poisoned with some kind of acetylcholinesterase. In terms of the heart, there is sinoatrial node suppression. So patients often presented with a decreased heart rate or what we call negative chronotropy and remember that Chronos was the God of time so decreased time means that these patients had a slower heart rate. In terms of the atria, there is decreased contractile force or negative inotropy. Inos was the Greek God of strength so there is less strength. In terms of the AV node, there is decreased conduction velocity of each impulse or negative dromotropy. 04:57 Dromos comes from the Greek root dromos, which means running, essentially signifying movement or speed. 05:03 So, things were going slower down a pathway. 05:06 Other effects on the AV node, an increased refractory period and in terms of the effect on the ventricles, there is decreased contractile force or negative inotropy. What are the cholinomimetic effects on the brain? So for example if you have a lot of nicotine, patients will have an elevated mood particularly alert and sometimes there is an addictive potential but if you're overdosing or if you're having toxic levels like in the sarin gas attack, patients would have a lot of nausea, a lot of vomiting, convulsions and even a coma. What about the effects on the circulatory system? You will generally get dilation of blood vessels, so there is a release of nitric oxide, originally known as endothelial derived relaxing factor, or EDRF, that dilates the blood vessels. 05:55 In terms of the lungs, you have the opposite, which is bronchoconstriction. 05:59 Remember that, because generally speaking, what the lungs are doing, the body does the opposite because of the way that the nervous system is set up. 06:07 So you have dilation of the peripheral circulation and constriction in the respiratory circulation, as well as bronchoconstriction. 06:15 In terms of the gut, you would have smooth muscle contraction, so you would have increased peristalsis. 06:24 In terms of the sphincters, you would have a contraction of the GE sphincter and a relaxation of the pyloric sphincter. 06:34 So that's kind of a hard thing to recognize until you realize what we're talking about here is moving things through quickly. 06:41 So the GE sphincter should contract because you don't want food to go back up into the stomach when the intestines contract. 06:49 That's how it's easy to remember. 06:52 In terms of the urinary tract, it's quite similar. 06:55 The detrusor muscle will contract, whereas the trigone will relax. 07:00 That ends up causing the bladder to open up its sphincter, contract, and push out urine. 07:07 The skeletal muscle effects of cholinomimetics occur by blockade of neuromuscular end plate function, which can be achieved by two basic mechanisms, either by nondepolarizing or depolarizing neuromuscular blocking drugs. 07:22 Examples of nondepolarizing neuromuscular blocking drugs include rocuronium, cisatracurium, vecuronium and atracurium, while D-tubocurine is the prototype of this group but is no longer used clinically. 07:36 Rocuronium has a rapid onset, making it ideal for rapid sequence intubation. 07:41 Cisatracurium is eliminated independently of organ function, which makes it useful in patients with organ impairment. 07:48 Vecuronium has an intermediate duration and causes minimal side effects. 07:52 Rocuronium and vecuronium, both aminosteroids, can be effectively reversed with sugammadex. 07:57 motor end plate. Blocking without activation. Unlike depolarizing agents like succinylcholine, rachuronium blocks these receptors without activating them, prevents the influx of sodium ions required for muscle contraction. 08:10 Reversible blockade, the neuromuscular block induced by rachuronium is reversible by increasing acetylcholine levels at the neuromuscular junction. Typically uses acetylcholinesterase inhibitors, such as neostigmine or edrophonium. The inhibitors increase acetylcholine concentration and outcompete rachuronium for receptor binding, so the blockade is reversed. The uses are facilitate endotracheal intubation, provide muscle relaxation during surgery, aid in mechanical ventilation by reducing muscle movement. Treatment for overdose or adverse effects, anticholinesterase inhibitors, these increase acetylcholine levels at the neuromuscular junction, helping to overcome the blockade caused by rachuronium, e.g. 08:55 neostigmine, edrophonium. Supportive care. In cases where respiratory muscles are affected, mechanical ventilation may be required. Depolarizing neuromuscular blocking drugs work through a unique mechanism, with succinylcholine being the only clinically used agent in this category. 09:14 Mechanism, succinylcholine acts by mimicking acetylcholine and serving as an agonist at nicotinic acetylcholine receptors, leading to an initial depolarization of the muscle cell membrane. This causes brief muscle contractions, known as fasciculations. However, unlike acetylcholine, succinylcholine is not rapidly degraded by acetylcholinesterase. As a result, it causes prolonged depolarization of the muscle membrane. 09:39 This prolonged depolarization induces a phase 1 block, during which muscle fibers remain unresponsive to further stimulation, leading to muscle relaxation. With continued exposure, the receptors can become desensitized to acetylcholine, resulting in a phase 2 block, where the muscle end plate repolarizes but becomes less responsive, similar to the action of nondepolarizing neuromuscular blockers. Uses. Succinylcholine is typically employed in short surgical procedures, where quick recovery of muscle function is necessary. It is commonly used for rapid sequence intubation due to its quick onset and short duration of action. 10:18 Contraindications include burns, crush injuries, hyperkalemia, and neuromuscular diseases. 10:25 In these cases, upregulated receptors can lead to life-threatening hyperkalemic cardiac arrest. 10:30 Treatment for overdose or adverse effects. Time. 10:35 Succinylcholine's effects are generally short-lived, as it is rapidly broken down by plasma cholinesterase. Mechanical ventilation. 10:43 In case of respiratory muscle paralysis, mechanical ventilation may be required until the drug is metabolized and normal function resumes. Dantraline. If succinylcholine induces malignant hyperthermia, Dantraline is administered to decrease muscle metabolism and reduce heat production. 11:03 Organophosphates are nondepolarizing agents that are commonly used as pesticides, with examples including malathion and chlorpyrifos. They have also been employed as nerve gases in terror attacks, such as sarin. 11:18 Mechanism. Organophosphates work by inhibiting acetylcholine esterase, which leads to an accumulation of acetylcholine. This results in prolonged activation of acetylcholine receptors, causing overstimulation of both muscarinic and nicotinic receptors, leading to a variety of symptoms. Muscarinic symptoms. These include salivation, lacrimation, urination, diarrhea, emesis, vomiting, bronchorea, excessive mucus secretion in the lungs, bronchospasm, bradycardia, slow heart rate, and meiosis, constricted pupils. Nicotinic symptoms. These manifest as muscle fasciculations and weakness. Central nervous system symptoms. Exposure can lead to seizures, coma, and respiratory failure. Treatment. 12:10 Atropine is used to counteract the muscarinic effects caused by organophosphate poisoning. Pralidoxim, 2-P-A-M, reactivates acetylcholine esterase by removing the organophosphate bound to the enzyme, alleviating the neuromuscular symptoms. Supportive care. Mechanical ventilation may be necessary if respiratory failure occurs, and benzodiazepines can be used to control seizures. 12:36 Decontamination. It is crucial to remove contaminated clothing and wash the body thoroughly to limit further exposure. It is important to note that neostigmine and edrophonium are not used for treating organophosphate poisoning. 12:50 The standard treatments are atropine and pralidoxim, along with supportive care and decontamination measures. 12:57 In terms of the exocrine glands, the sweat glands will increase their production and release so you have more sweating, you have salivary gland hyperexcitation so you have more salivation, mouth is wet. The tear ducts are more stimulated so you have more lacrimation. And in terms of the GI and lung mucous glands, you have more secretion. So it's a hard thing to remember but just remember that what we're trying to do here is we're trying to make things wet. So patients are wet with cholinomimetics so therefore there is more sweat, more saliva, more tears, and more mucous from the mucous membranes. So, I have a mnemonic for you called DUMBELLS which is good for cholinomimetic. So D is diarrhea, urination, myosis, bronchoconstriction, bradycardia, excitation of skeletal muscle and central nervous system, lacrimation, salivation, and sweating. 14:01 Nicotinic and central nervous system effects can include muscle fasciculations, weakness, and paralysis. 14:08 Patients may develop tachycardia and hypertension. 14:11 In the CNS, symptoms range from confusion and seizures to coma, and severe cases can lead to respiratory failure.
About the Lecture
The lecture Cholinomimetic Activators and Effects by Pravin Shukle, MD is from the course ANS - Pharmacology.
Included Quiz Questions
All of the following effects would be expected in organophosphate poisoning EXCEPT...?
- ...hypertension.
- ...diarrhea.
- ...salivation.
- ...miosis.
- ...bradycardia.
What is NOT a potential use for acetylcholinesterase inhibitors?
- Muscle relaxant
- Pesticide
- Diagnosis of neuromuscular junction disease
- Chemical weapon
- Treatment for myasthenia gravis
What is the usual cause of death caused by sarin (acetylcholinesterase inhibitor)?
- Asphyxia
- Hemorrhagic shock
- Cardiac arrest
- Delusional state
- Brain edema
What is a commonly used antidote to control the muscarinic effects of organophosphate poisoning?
- Atropine
- Pralidoxime
- Leucovorin
- Flumazenil
- Benztropine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |