Playlist
Show Playlist
Hide Playlist
Cellular Response: Introduction
-
Slides Acute and Chronic Inflammation Cellular response.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
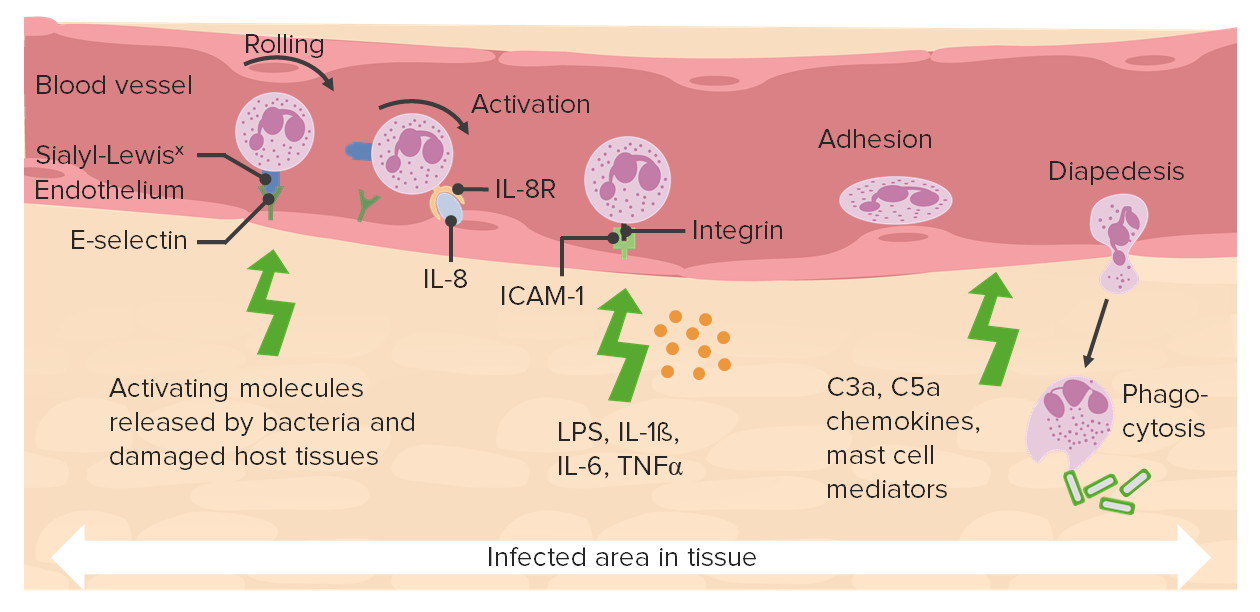
00:01 Welcome. 00:01 The topic for discussion is all about the cellular response in acute inflammation. 00:07 We've previously talked about the vascular response. 00:10 And now we're going to bring in the neutrophils. 00:13 The acute inflammatory cells that are going to clean up the mess that happened when we had injury and start the healing response. 00:24 The cellular response involves neutrophil recruitment, so getting them in to the area of injury. 00:30 Once they're there, they have to phagocytized, they have to eat, and they have to kill. 00:36 And they will also have mediators that they will release that will be important in this inflammatory response. 00:43 Those mediators include reactive oxygen species, that we've talked about before, ROS. 00:47 ROS are very important in this process. 00:50 And we'll cover that in detail. 00:52 They also elaborate proteases to degrade the debris that has been part of the injury in that location. 01:00 And they will elaborate a number of other mediators, including importantly eicosanoids. 01:05 And we'll spend a fair amount of time talking about eicosanoids. 01:09 There are lots of details here. 01:11 There are lots of very important things that we will be interested in. 01:16 So hang in there, keep in mind, these basic kind of buckets of what we're going to talk about. 01:23 The first thing is getting the neutrophils in to the tissue of the area of injury. 01:28 So this is our vascular bed. 01:29 We have coming from the left side into the right side, we have arteriole that branches into capillaries, that then comes into back together into the postcapillary venule. 01:40 There are a few cells that are normally in the extravascular matrix, lymphocytes, and macrophages. 01:48 There will also be mast cells and other tissue types of cells. 01:53 When we have acute inflammatory responses in response to injury, what we've already discussed is that increased vascular flow. 02:03 so we have dilation of the arteriole and increase flow into the tissue. 02:08 This provides greater blood into the area of injury. 02:12 The entire bed of vessels gets more dilated. 02:16 So that will be apparent grossly as calor (heat), and rubor (redness). 02:23 And there will also be increased vascular permeability, as we've talked about, as we increase the hydrostatic pressure. 02:29 We've also now in this vascularized area of cellular inflammation, we've recruited and have neutrophils that have left the blood vessels and are in the tissue. 02:40 And they are looking around, for where's the damage, and how can they help clean it up? So the next process that we're going to talk about is, how do we get the neutrophils there? This is going to be a complex kind of animation that we will walk through to look at how neutrophils, and other inflammatory cells can lead the bloodstream, and get into the area where there has been injury. 03:08 So what we're looking at essentially is the endothelium, that's that yellow line near the bottom, it sits on a basement membrane and below it is the extravascular matrix. 03:17 And above that in the bloodstream, would be a leukocyte. 03:20 And we're going to have blood flow going from right to left. 03:24 So, what we have here is a leukocyte not at surface or a variety of molecules, those will become important in a minute. 03:31 Okay. 03:32 We need to somehow tell the leukocyte, "Come here. Dive into this spot." And that involves cells that are acting as sentinels that live in the extravascular space, mast cells, and macrophages, will respond to injury. 03:48 And we'll talk about how that happens. 03:50 But we'll respond to injury and make a variety of mediators that will turn on the endothelium and make it sticky. 03:57 And that will be a cue to the leukocytes that this is where they need to go. 04:02 Macrophages and mast cells are also going to make the vessels leakier. 04:06 So the endothelium will pull slightly apart and we will get fluid that comes out. 04:10 As a result of that, we get stasis. 04:13 We get a relative sluggishness of the blood because a lot of the extra water and electrolyte has flowed out into the tissue. 04:20 That's the tumor that we talked about previously, the edema, that's associated with the vascular response. 04:26 By making the blood flow sluggish, now those leukocytes that are zipping by start bouncing along the surface of the endothelium. 04:36 That's the next step, that's rolling. 04:38 And we'll talk about how the various molecules on the endothelium and on the leukocyte are involved in that rolling process. 04:46 The leukocyte will roll for a while and then driven by additional molecules chemokines that you see there, the leukocyte molecules undergo changes that allow them to get really very sticky, and you finally get them to have firm stable adhesion. 05:06 They layer down, and now, again driven in part by the chemokines, they will crawl across. 05:12 The crawl across the endothelium into the space where the injury has occurred or where the infection is happening. 05:19 And then they will follow gradients that say, "Over here. This is where you want to go." That's where the infection is. 05:26 And they will use the extracellular matrix to crawl. 05:31 And they will get to the spot where they then are going to elaborate their mediators, and they will eat, they will phagocytize. 05:37 So this process, multiple stages, a lot of important molecules that are involved, and there are therapeutic opportunities throughout this. 05:45 So we'll come back to each of these individual stages.
About the Lecture
The lecture Cellular Response: Introduction by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Which of the following mediators is produced by neutrophils during acute inflammation?
- Reactive oxygen species
- Histamine
- Complement component C3b
- Immunoglobulins
- von Willebrand factor
What is the correct order of the stages of neutrophil migration during acute inflammation?
- Rolling, integrin activation, stable adhesion, migration through the endothelium
- Rolling, integrin activation, stable adhesion, stasis, migration through the endothelium
- Vasoconstriction, rolling, integrin activation, stable adhesion, migration through the endothelium
- Integrin activation, rolling, stable adhesion, migration through the endothelium
- Stable adhesion, rolling, integrin activation, migration through the endothelium
Which of the following changes takes place in the capillary bed during inflammation?
- Arteriolar dilation
- Decreased vascular permeability
- Venular constriction
- Contraction of the capillary bed
- Increased intravascular oncotic pressure
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |