Playlist
Show Playlist
Hide Playlist
Case: 45-year-old Man with Bilateral Lower Extremity Weakness and Numbness
-
Slides Diseases of the Spinal Cord.pdf
-
Download Lecture Overview
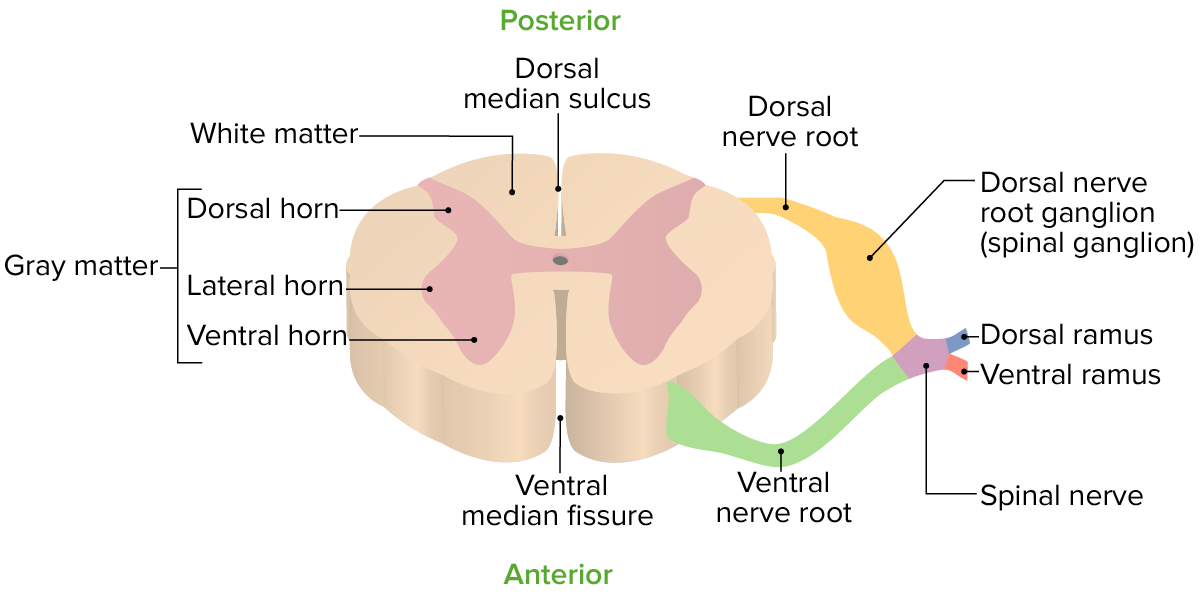
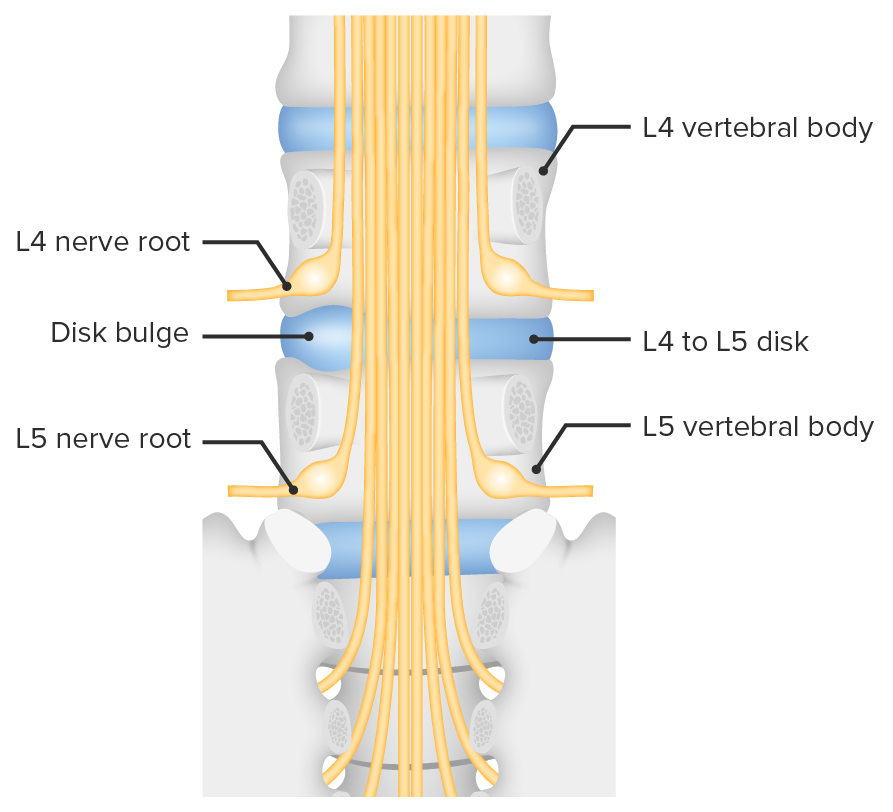
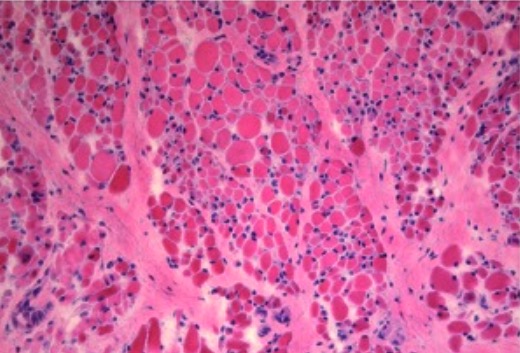
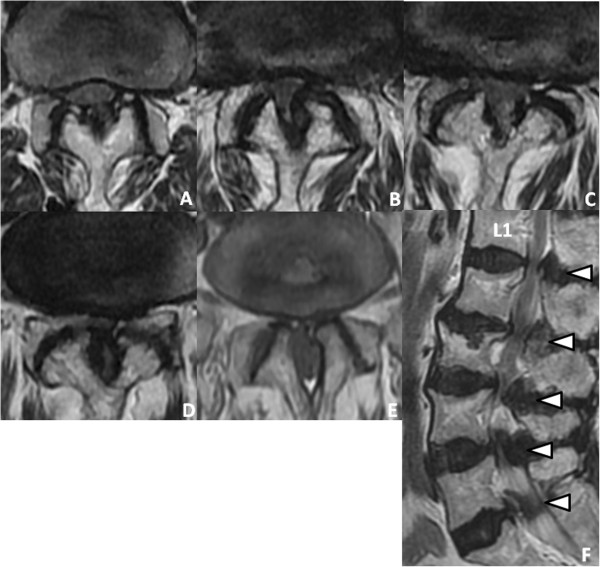
00:00 In this talk, we're going to discuss spinal cord disorders. This is a really important talk. 00:07 We see a lot of different presentations from spinal cord pathology but if you can break it down and figure out where in the spinal cord the problem is, it becomes much easier to approach these patients in either a case or a question. So let's start with an introduction to spinal cord disorders and diseases, and let's begin with a case. This is a 45-year-old who awoke with bilateral lower extremity weakness and numbness which resolved over several days. Over the next few weeks, he developed back pain and gradually progressive urinary retention and constipation. Lumbar spine MRI showed mild degenerative changes and he subsequently developed genital numbness and sexual dysfunction. Inflammatory myopathy was initially suspected and corticosteroids were administered, but within 12 hours he suddenly developed bilateral paraparesis meaning weakness and numbness below the waist and severe worsening of his symptoms. Exam now shows 2/5 strength in the bilateral lower extremities. He can't achieve at least antigravity strength in the legs; hyperreflexia in the bilateral lower extremities; and bilateral Babinski signs, evidence of upper motor neuron dysfunction. 01:25 Sensory exam shows reduced pinprick, temperature, and vibration in the legs. Upper extremity examination is normal. So let's walk through some of the key features of this case that guide us to where the problem is and what the localization is for this patient. The first is the strength exam. This patient has significant bilateral relatively symmetric weakness in the legs. That's a paraparesis or weakness and often numbness below the waist, and this is strongly indicative of a spinal cord disorder. The 2nd is the reflex exam, which is really important in this case. Reflexes are some of the most objective portions of our exam and here the presence of bilateral hyperreflexia points to an upper motor neuron disorder and squarely sets this in the spinal cord. The last is the sensory exam and we have diffuse sensory dysfunction to pain and temperature with pinprick and temperature reduction as well as vibration and proprioception with reduced vibration in the bilateral legs. And we really want to interrogate in this patient whether there is a sensory level, which would also be supportive of a spinal cord disorder. And the last is a unique wildcard in this case, which is very rare, and must be something to focus in on when you see it, and this patient had sudden worsening of symptoms with initiation of corticosteroids. Steroids are one of those medicines we use in neurology and medicine to help just about any problem. They can help inflammatory disorders and some infectious disorders, and in paraneoplastic disorders but there is dramatic worsening in this patient with the initiation of steroids and this tips us off that this may be vascular in origin. So, what's the localization? Where is this problem? Is it in the brain, the subcortex, brainstem, or spinal cord? Well, this isn't a presentation of a brain disorder. There's no cortical symptoms, no abnormality in mental status. The mental status exam was essentially normal and not mentioned because of its normality in this patient and this is not the presentation of brain pathology. Similarly, there is nothing pointing us to something in the subcortex. 03:35 The symptoms and deficits involved both legs, and the motor and sensory fibers to the legs are different, they're in opposite sides, opposite hemispheres of the brain in the subcortex. It would take a really large lesion to affect both legs and the motor and sensory fibers for both legs and we would surely see problems with mentation or other brain symptoms or signs in these patients and this is inconsistent with the presentation from the subcortex. We also don't see things that point us to the brainstem. They're not crossed findings or cranial nerve dysfunction and nothing else that points us to brainstem pathology. And this is the classic presentation of someone with a myelopathy or a spinal cord disorder. A paraparesis, upper motor neuron reflexes, and the presence of a sensory level would seal the deal on a myelopathic process. In this patient, the patient underwent MRI of the spine which is a critical diagnostic test that we'll find in evaluating these patients and here in A we're looking at a T2 image and this shows the spinal cord is dark and any pathology shows up is bright. And we can see throughout the thoracic spine there is increased signal hyperintensity, white signal within the spinal cord from, in this case, a venous hypertension. Some pathology is present in the spinal cord and that's what's causing this patient's symptoms. In B, we're looking just lateral to the spinal cord and we see this area of flow void, dark signal within the spinal fluid that is suggestive of an enlarged blood vessel. This patient went on to have a spinal angiogram, which you can see in C and D and we have a large vein arising from an artery, a medullary branching artery in to the spinal cord and that vein is the problem. 05:17 It is a connection between the artery and a vein. It results in venous hypertension or back-up of blood within the venous flow of the spinal cord, and that's what that signal is so that we're seeing the spinal cord is venous hypertension, too much blood in the veins spilling into the spinal cord. And this is the classic imaging of a spinal dural AV fistula, which was the cause of this patient's chonical symptoms and one of those unique disorders that worsens with corticosteroid administration.
About the Lecture
The lecture Case: 45-year-old Man with Bilateral Lower Extremity Weakness and Numbness by Roy Strowd, MD is from the course Diseases of the Spinal Cord.
Included Quiz Questions
Which of the following is a sign of an upper motor neuron lesion?
- Hyperreflexia
- Hyporeflexia
- Flaccidity
- Negative Babinski sign
- Fasciculations
What is the best diagnostic tool to identify myelopathy?
- MRI
- CT scan
- X-ray
- Lumbar puncture
- Electromyography
Which of these is the correct localization of symptoms for a CNS lesion?
- Spinal cord–bilateral decreased motor strength, hyperreflexia, and a sensory level
- Brain stem–mental status changes
- Subcortex–motor symptoms in both lower extremities with upper extremities unaffected
- Brain–cranial nerve dysfunction and bilateral leg weakness
- Spinal cord–hemiparesis and altered mental status
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |