Playlist
Show Playlist
Hide Playlist
Interpretation of Serum Calcium and Serum Phosphate Levels
-
Slides VitaminDPathologies EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
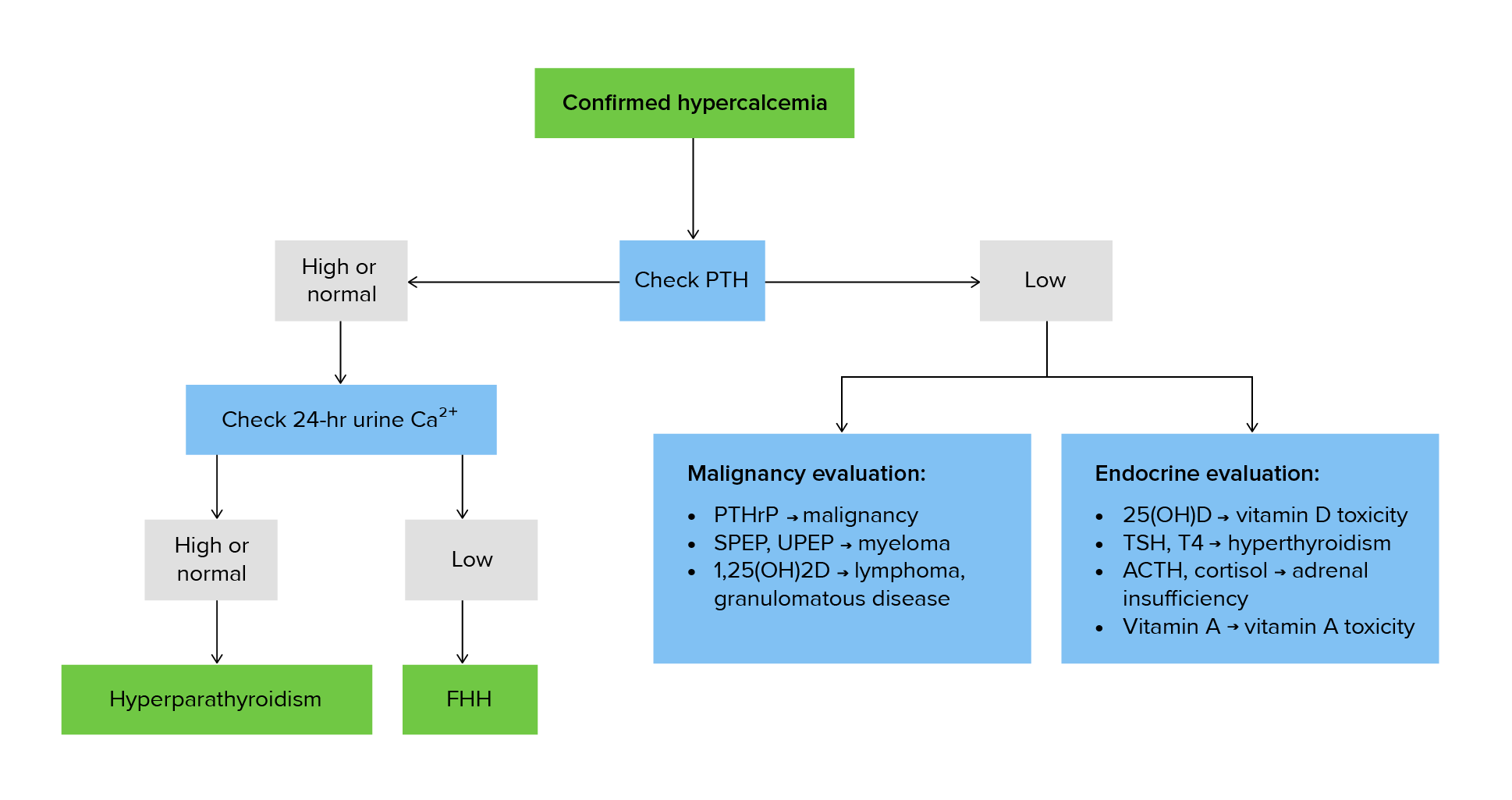
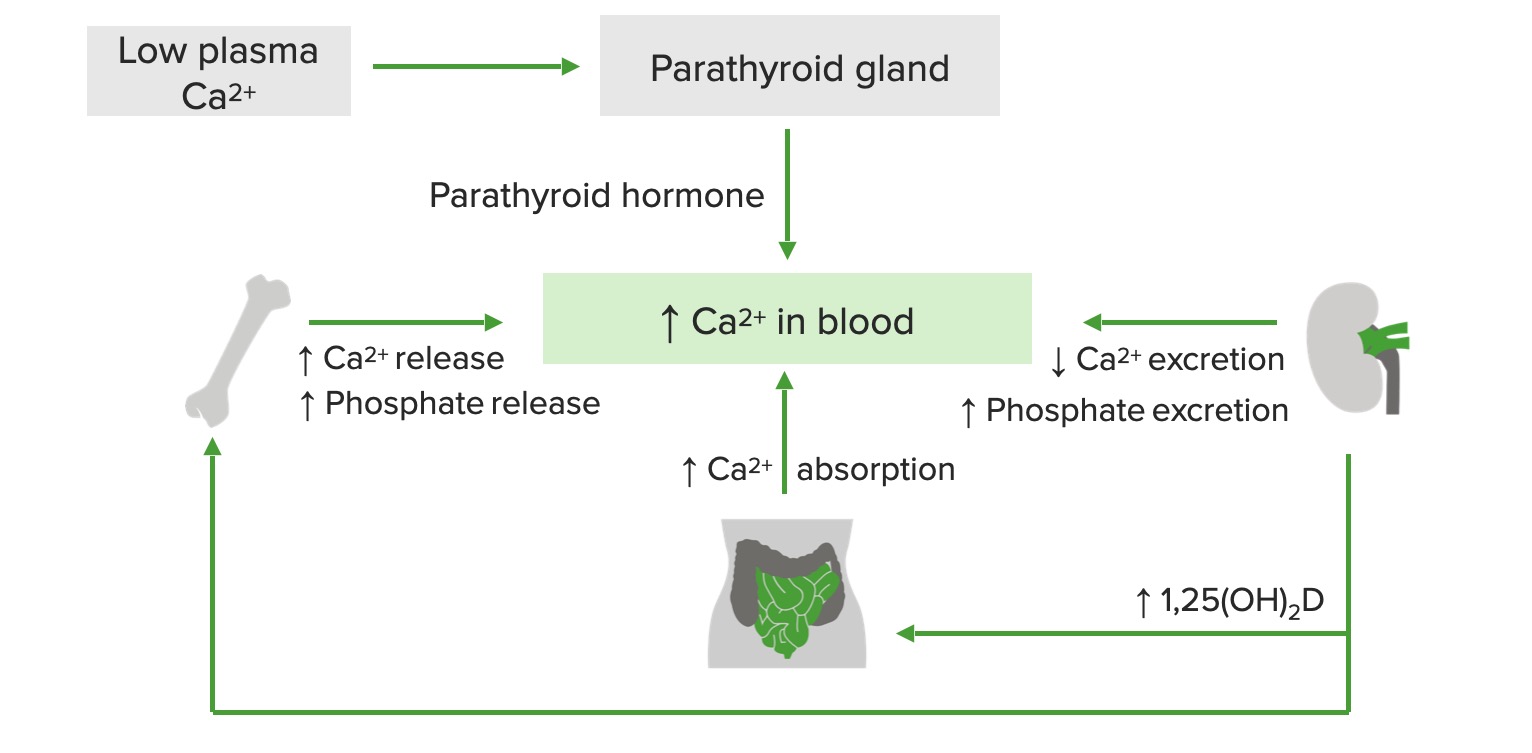
00:02 Simplified Calcium/Phosphate interpretation. 00:05 Low Vitamin D action, low calcium and we have low phosphate, unless renal failure. 00:13 I’ve emphasized that so many times now. 00:16 Whenever you have calcium imbalance, you’re always going to look for renal status, always. 00:23 It changes the entire complexity or complexion of the pathology. 00:28 If it’s high Vitamin D action, the opposite would be true. 00:33 If it’s low PTH action, why? Well, maybe the hyperparathyr-... the parathyroids have been lost resulting in low PTH action. 00:44 You would expect there would be low calcium and high phosphate. 00:48 If there’s high PTH or PTHrp and with this, we’ve talked about with primary hyperparathyroidism or secondary hyperparathyroidism, once again, the big exception here, we expect your calcium to be high, your phosphate will be low because PTH gets rid of your phosphate, unless renal failure where the phosphate will be elevated. 01:13 Bottom line, calcium and phosphate tend to deviate together, both up or down, in Vitamin D derangements whereas the deviation or the changes between calcium and phosphate will be the opposite when it comes to parathyroid pathologies, generally. 01:34 Exception, chronic… a big exception, chronic renal failure.
About the Lecture
The lecture Interpretation of Serum Calcium and Serum Phosphate Levels by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
What are the expected labs in a patient with chronic renal failure and low vitamin D?
- Decreased serum calcium, increased serum phosphate
- Decreased serum calcium, decreased serum phosphate
- Increased serum calcium, decreased serum phosphate
- Increased serum calcium, increased serum phosphate
- Normal serum calcium, decreased serum phosphate
A patient presents with increased serum calcium and decreased serum phosphate. What is the most likely cause of this electrolyte imbalance?
- Elevated PTHrP
- Low PTH action
- Low vitamin D action
- Elevated vitamin D action
- Chronic kidney disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Best professor in lecturio make him make more lectures please
Easy to understand and remember. Straight to the point where students mostly get confused