Playlist
Show Playlist
Hide Playlist
C. Difficile Infection (Antibiotics)
-
Slides InfectiousDiarrhea InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
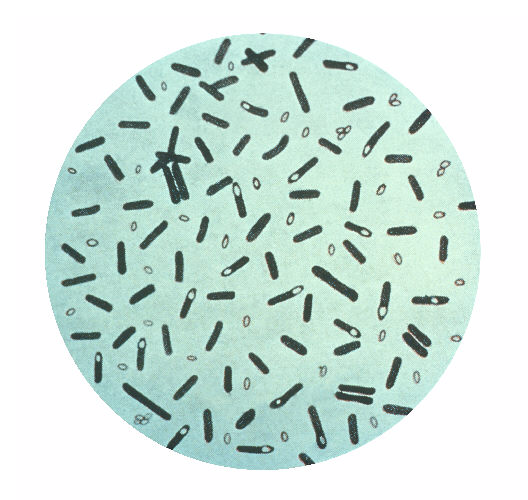
00:00 Now let's talk about the antibiotics that we need to worry about. The ones that seem to be frequently linked to antibiotic-associated colitis are ampicillin and amoxicillin, the cephalosporins, the clindamycin and particularly the fluoroquinolones and these organisms are fairly broad spectrum. Less frequently, we talk about the tetracyclines, sulfonamides, erythromycin. We don't use much chloramphenicol in the United States anymore and trimethoprim and I'll start out by saying that I have never recognized antibiotic colitis due to an aminoglycoside. The aminoglycosides like gentamicin essentially only hit aerobic gram-negative rods for all practical purposes and it must be as rare as hen’s teeth for metronidazole to cause antibiotic colitis because metronidazole and vancomycin are two of the treatments we use to kill C. difficile. 01:18 So I've never seen it but it's on the list as a rare cause. Now this organism, Clostridioides difficile, like other Clostridia is a spore-forming organism. So when it falls upon hard times even in the intestine, it may form spores which allow it to survive under environmental circumstances that are unfavorable to the organism and it's these spores that can be ingested and also can disseminate and that dissemination sometimes takes place even in the hospital and they can colonize the surface when antibiotics have altered their colonization resistance. So let's say somebody is receiving an antibiotic that even works against Clostridioides difficile or the organism may form spores and the spores are essentially impervious even to antibiotics that kill C. difficile. So in the hospital, if someone has antibiotic colitis caused by this bacterium, we need to isolate the patient so barrier precautions are needed. So this organism makes essentially 3 toxins. It makes an A toxin, TcdA, which would be toxin of C. difficile A. 02:52 TcdB and it's really the B toxin that's the bad boy, it's a thousand times more potent than the A toxin and then it makes a binary toxin that is very mild in terms of its effect on the GI mucosa. 03:14 So what the toxin does is it glycosylates and inactivates GTPases and GTPases are enzymes which control actin cytoskeleton of cells. If you disrupt the actin cytoskeleton, you're going to kill the cell. You also, in killing the cells, disrupt the barrier function of the mucosa and the cells either directly are killed or they become apoptotic and it's no surprise that you get an inflammatory response with an infection caused by C. difficile. So the toxins enter the cytoplasm. They then glycosylate the RhoB protein, which is the regulator of the actin cytoskeleton. They disrupt the actin cytoskeleton and kill the cell. So let's talk about the spectrum of disease. The expression of the disease how severe it is depends upon the host's susceptibility or the immunity. Some strains are more virulent than others and the timing and the type of antibiotic therapy, for instance if you started somebody on ampicillin and they received a short course, well C. difficile may try to overgrow but after stopping the antibiotic, the other organisms come back quickly and the diarrhea resolves spontaneously. It was due to C. difficile but it was self-limited. So, the other thing is that antibiotic-associated diarrhea may have other causes. You can also carry C. difficile as I like to say the students down there in the dark asymptomatically. I would guess a sizable minority of us have this organism, maybe 30% of us have this organism in our intestine now. Then there's the diarrhea that starts the C. difficile associated diarrhea and if it's progressive it will become pseudomembranous colitis and it can result in fulminant colitis with toxic megacolon and death. 05:59 So how do you diagnose antibiotic-associated colitis. 06:03 We use the two-step diagnostic testing method. 06:06 It's crucial to note that testing should only be performed on liquid stool samples from patients with symptoms suggestive of CDI. 06:14 Step one involves two simultaneous tests: Glutamate Dehydrogenase or GDH, which screens for the presence of C. difficile and toxin EIA, which detects toxicgenic C. difficile and supports the diagnosis of CDI. 06:29 Step two comes into play only with discordant results. 06:33 Let's walk through the interpretation algorithm. 06:36 When both GDH and toxin are positive, this confirms CDI. 06:41 However, if we find a positive GDH but negative toxin, we move to step two - Nucleic Acid Amplification Testing or NAAT. a positive NAAT in this scenario could indicate either active infection or simply colonization. 06:57 This is where clinical correlation becomes essential. 07:00 If the NAAT is negative, we can rule out CDI. 07:04 If we encounter a negative GDH but positive toxin, this represents a technical error and requires repeat testing. 07:11 Finally, if both initial tests are negative, we can confidently rule out CDI. 07:16 Remember, these tests should never be used for test of cure and clinical symptoms must always guide our interpretation of results. 07:24 Now if the diagnosis remains in doubt, or they are no better with treatment then s CT abdomen/pelvis with contrast should be done to evaluate for toxic megacolon or bowel perforation. 07:37 A lower GI endoscopy has a high perforation risk, but may be necessary to rule out an alternative diagnosis. 07:45 Thats were we see pseudomembranous colitis. Now, they call it pseudomembranous colitis, it's a very adherent not pseudomembrane, not a real membrane, composed of white cells and the sloughed mucosal epithelium. That's what you're looking at. 08:06 So how do we manage antibiotic associated colitis? Well, if the initial episode is mild or moderate, with a white cell count less than 15,000 and normal renal function, the recommended treatment is either oral vancomycin or oral fidaxomicin If neither of these drugs are available metronidazole can be given. 08:25 If the case is more severe, with a white cell count over 15,000 and reduced renal function, the same first line treatments are recommended, but oral metronidazole is no longer considered an appropriate treatment. 08:37 If the patient goes on to develop hypertension, shock, or develops an ileus, we can escalate treatment to oral vancomycin plus IV metronidazole If the ileus is present, we can consider rectal administration of the vancomycin as well as a fecal microbiota transplant. 08:54 If the infection recurs, your antibiotic selection is determined partially by the previous treatment. 09:00 If vancomycin was initially used, you can try pulse-tapered vancomycin, or fidaxcomicin. 09:05 If on the other hand, vancomycin was not used for the initial infection, it will become the first-line treatment for the recurrence. 09:12 If the patient develops a second recurrence, your choices would be either pulse-tapered vancomycin, fidaxomicin, vancomycin followed by rifaximin, or a fecal microbiome transplant. 09:25 What's really promising in the treatment of particularly severe or recurrent C. difficile infection is giving. I know it sounds terrible, a fecal transplant from people who donate normal stool. 09:45 And the idea is that normal stool contains other bacteria, that once they get into the colon, will quiet down the growth of C. diff. 10:00 And initially, the way to give it was not very satisfactory. 10:06 We'd give it through a colonoscope by retention enema. 10:11 Or actually put feces down a nasogastric tube. 10:18 Or there are now some oral capsulized frozen fecal samples that we can give like a pill. 10:27 And believe it or not, as strange as this might sound, and they are highly effective in preventing multiple recurrences. 10:37 91% efficacy. 10:40 Although fecal transplants are efficacious, there is the danger of transmitting multi-drug-resistant pathogens. 10:46 Other therapies include a monoclonal AB against the B toxin, bezlotoxumab, which is available to decrease recurrences but is very expensive. 10:57 So, I think, the trend now is to figure out a way to do this more aesthetically pleasing. 11:06 And the things that are uncertain are what actually organisms in feces, do the protection? We don't know that. 11:17 And there are some experimental things by Series Health Ser-109. 11:23 It's a combination of bacterial spores in pill form And, it's not ready for primetime but it's promising for recurrent C. diff infections. 11:35 So, that's a lot about C. difficile, but it needed a lot of discussion because of the importance of this in modern medicine.
About the Lecture
The lecture C. Difficile Infection (Antibiotics) by John Fisher, MD is from the course Gastrointestinal Infections.
Included Quiz Questions
Which of the following antibiotics is LEAST likely to be the cause of antibiotic-associated colitis?
- Vancomycin
- Ampicillin
- Amoxicillin
- Clindamycin
- Trimethoprim
A patient has a second relapse of C. difficile colitis due to spore formation. What is the appropriate treatment?
- Pulsed regimen of oral vancomycin
- High dose intravenous vancomycin
- Intravenous metronidazole
- Oral metronidazole
- Oral metronidazole plus rectal vancomycin
How is C. difficile transmitted?
- Fecal-oral route
- C. difficile is not contagious, it is only due to antimicrobial treatment
- Through aspiration of spores
- Through ingestion of contaminated foods
- Typically spread through surgical instrumentation
Which C. difficile toxin is the most potent?
- Tcd B
- Tcd A
- Subunit C
- Binery Toxin
- CDT
How does the C. difficile toxin affect cells of the colon?
- Enters the cytoplasm and glycosylates RhoB protein which disrupts the actin cytoskeleton and kills the cell
- Binds to GM1 ganglioside on the mucosal cell surface and enters the endoplasmic reticulum
- Binds to Rho B protein then creates a pore in the cell wall and allows the active toxin to enter the cytoplasm
- Enters the cytoplasm and increases the production of cyclic AMP which causes ion transport abnormalities
- Enters the cytoplasm and is transported into the mitochondria through RhoB receptors which promotes an inflammatory response and cellular apoptosis
How is the diagnosis of C. difficile colitis typically confirmed?
- Enzyme immunoassay of 2 stool specimens
- It is simply a clinical diagnosis
- Serum analysis for C. difficile toxin A
- It can only be confirmed by pseudomembrane biopsy
- Stool cultures
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |