Playlist
Show Playlist
Hide Playlist
Major Burns: ABC Management
-
Emergency Medicine Burns.pdf
-
Download Lecture Overview
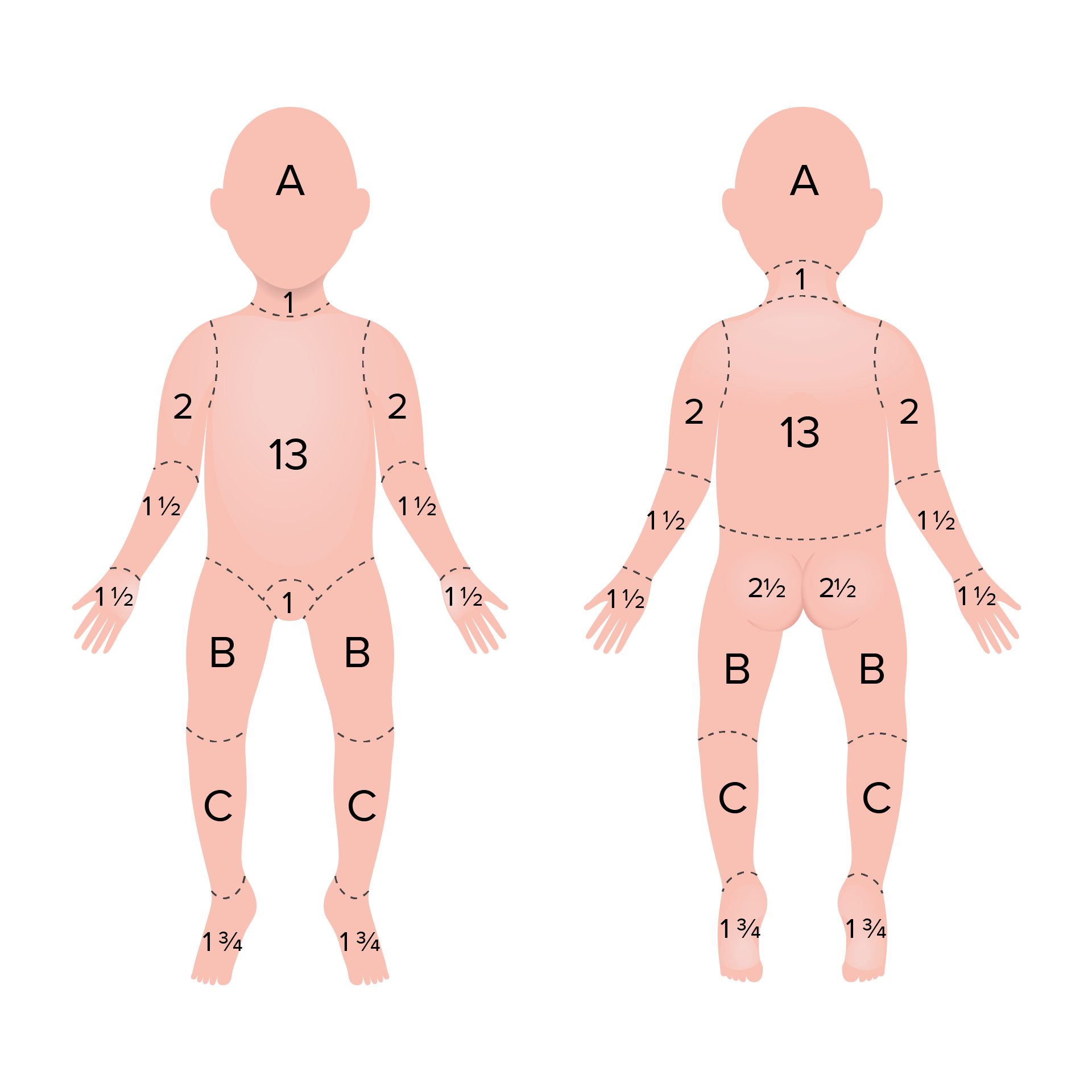
00:01 So those are cutaneous burns. 00:03 But remember, burns don’t just happen on the skin. 00:05 They can happen anywhere in the body. 00:07 And one of the places we need to be very, very concerned about burns are in the airway. 00:12 So airway burns can cause death due to edema and airway obstruction, and you really wanna be very aggressive about managing the airway in patients who do have evidence of airway burning, because if they are obstructed a little bit when you meet them, there’s a good chance that they’re gonna swell more, and become more obstructed as time goes on. 00:33 Please also look for indicators of future airway loss. 00:39 So signs of airway obstruction immediately right now would include stridor. 00:44 Just as a reminder, stridor is a high-pitched inspiratory sound that’s made because air is being forced through a very narrowed opening. 00:54 So that’s what stridor sounds like. 00:58 With each inspiration. 00:59 You'll also also see pharyngeal swelling. 01:01 When you look into the airway, and the patient typically has some degree of respiratory distress. 01:06 If any of those things are present, you definitely gonna wanna intubate right away. 01:11 You also wanna look for indicators of future airway compromise. 01:14 So those might include burns around the face or mouth. 01:18 Singed nasal hair. 01:20 Soot in the mouth or carbonaceous sputum, so when the patient coughs, they produce sputum that’s black in color and any kind of voice changes. 01:28 These should all be considered harbingers of potential compromise of the airway down the line. 01:34 Now, one thing I do wanna emphasize is it's a little bit problematic with airways and burns is that a lot of patients who have these traditional indicators of future airway compromise will not end up having any airway injury. 01:48 And there are patients who have documented airway injury who lack these findings at presentation. 01:53 So it can be a little bit unreliable to assess for a future airway loss. 01:59 So you wanna be aware of the limitations of your clinical exam. 02:04 Now, we don’t wanna go just intubating everybody, because overly aggressive intubation can lead to its own complications including ARDS, barotrauma, ventilator-associated pneumonia, etcetera. 02:17 So we definitely want to assess the airway whenever we can using direct visualization of the airway either with the larynges scope, a video larynges scope, a fiber optic scope, etcetera. 02:29 Now, hopefully, if you are the emergency physician caring for this patient, you’ll have the technical expertise to manage the patient’s airway on your own, but these are often difficult airways. 02:40 So if you don’t have a lot of experience with airway management or if you are in a setting where you don’t have a lot of equipment that you can use to help manage a failed airway, get anesthesiology or otolaryngology involved to help you assess and manage the airway whenever possible. 02:57 All right. 02:57 So we addressed A, let’s talk about B. 03:00 So there are a number of ways in which burns can affect breathing. 03:04 In particular, you can have thermal burning of the lung tissue when you inhale superheated air in a fire, and you can also have smoke inhalation which can lead to a carbon monoxide poisoning. 03:17 When we manage patients who have respiratory compromise from burns, we wanna give them oxygen to make sure that we keep their stats above 92%, and we wanna humidify that oxygen because a lot of times patients who do have thermal burning of the lungs will find it much more comfortable to breathe air that’s a little wet as opposed to air that’s dry. 03:39 We definitely wanna use inhaled beta agonists like albuterol for bronchoconstriction and whizzing, and we do wanna consider intubation and mechanical ventilation for any patient who is significantly hypoxic despite supplemental oxygen. 03:53 For any patient who has significant respiratory distress or signs of respiratory failure, and of course for patients who have head injuries or other complications of their burns that have depressed their GCS, and in those cases the goals is gonna be protection of the airway. 04:10 Now, remember it’s not only thermal burning of the lungs we have to be concerned about. 04:14 It’s actually poisoning with carbon monoxide that occurs through inhalation of smoke. 04:19 Carbon monoxide is a real problem at the cellular level because what it does is it binds avidly to hemoglobin displacing oxygen from hemoglobin and creating a really tight bond with the hemoglobin molecule. 04:33 That means that oxygen can’t be effectively delivered to tissue so this causes tissue level hypoxia. 04:40 You always wanna measure the carboxyhemoglobin directly it's a laboratory assay that’s readily available in most hospitals, and you should never rely on your oxygen saturation to assess for carbon monoxide toxicity because actually, it will be falsely elevated. 04:56 So conventional pulse oximeters read carboxyhemoglobin as a saturated hemoglobin. 05:03 So your patient might have very, very poor tissue level oxygen delivery but their pulse ox waveform is gonna be saying a 100%. 05:12 and you wanna really be careful about that. 05:14 So again, measure the carboxyhemoglobin. 05:17 Anytime you’re dealing with carbon monoxide poisoning, your first line treatment is gonna be high flow oxygen. 05:23 You wanna get as close as you can to a 100% FIO2 either using a mask or using an endotracheal tube, depending on the patients' overall clinical status. 05:33 High flow oxygen will help displace the carbon monoxide from the hemoglobin allowing oxygen to bind back on to the hemoglobin binding sites and ultimately be delivered to tissue. 05:44 Oxygen also reduces the half-life of carbon monoxide and allows you to clear it by getting it off of the hemoglobin. 05:51 If regular high flow oxygen isn’t enough, you can consider hyperbaric oxygen. 05:56 Now, treatment in hyperbaric chamber is never been shown to offer any mortality benefit for burn victims. 06:02 However, it does potentially reduce the risk of not long term neurologic sequelae from carbon monoxide poisoning so you can consider it in certain cases. 06:12 It’s of greatest benefit when it’s begun within six hours of the burn. 06:16 So if you’re gonna do it, you wanna make sure that you initiate the necessary process to transfer your patient to a hyperbaric center as soon as possible. 06:27 You should think about hyperbaric oxygen when your patient has a carboxyhemoglobin of greater than 25%. 06:33 That is a lot of carbon monoxide and their hyperbaric oxygen is gonna help them clear it more quickly and hopefully help them have fewer complications from it. 06:43 Anytime you have a pregnant patient who has a carboxyhemoglobin of greater that 15%, you should also think about of hyperbaric oxygen in that setting, because the unborn fetus is much more sensitive to tissue level hypoxia than the adult is, because tissues are not yet fully formed, etcetara. 07:02 You also can think about hyperbaric treatment for patients who have clinical evidence of carbon monoxide toxicity. 07:10 So if they are comatose or their mental status is altered, if they are seizing, if they’re showing evidence of cardiac ischemia or arrhythmias. 07:18 These are all situations where you can think about using carboxyhemoglo — I’m sorry, using hyperbaric oxygen to try to displace carbon monoxide from the hemoglobin and restore tissue level perfusion. 07:34 Moving on to C, circulation is a really important issue in major burns because patients who have significant surface areas of their body burned can have a lot of insensible fluid loss and a lot of third-spacing of fluid that’s supposed to be in the intravascular space. 07:52 So you’ve got to really keep very close tabs on this patient’s volume status and aggressively treat hypovolemia and tissue level hypoperfusion. 08:02 Any patient who has a burn greater that 20% total body surface area or greater than 10% for children is gonna need careful fluid resuscitation. 08:13 And that’s typically done using formulas that allows to compute the fluid losses associated with burns. 08:21 All of these patients should have two large-bore IVs or central IV access to make sure that you’ve got a way to give them fluids rapidly and reliably, and we’re gonna base our calculation of how much fluid they need on their total body surface area.
About the Lecture
The lecture Major Burns: ABC Management by Julianna Jung, MD, FACEP is from the course Toxicologic and Environmental Emergencies. It contains the following chapters:
- Airway Management in Major Burns
- Managing Breathing in Major Burns
- Managing Circulation in Major Burns
Included Quiz Questions
In the examination of a burn patient, what breath sound will indicate a possible airway obstruction?
- Stridor
- Rhonchi
- Crackles
- Wheezing
- Decreased breath sounds
What is the mechanism of carbon monoxide poisoning?
- Carbon monoxide has a much higher affinity than oxygen for the same binding sites on hemoglobin.
- Direct trauma to lung tissue
- Decreases ventilation
- Prevents oxygen from being released by hemoglobin
- Prevents carbon dioxide from being excreted
What is the first-line treatment for carbon monoxide poisoning?
- 100% oxygen via mask or ETT
- Hyperbaric oxygen
- Orotracheal intubation
- Hyperventilation
- Blood transfusion
At what CO-Hgb percentage is hyperbaric oxygen recommended in non-pregnant patients, preferably within 6 hours?
- > 25%
- > 5%
- 5–10%
- > 10%
- 10–20%
At what percentage of TBSA affected in adults is fluid resuscitation indicated?
- > 20%
- 5%
- 5–10%
- 10–15%
- 15–20%
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |