Playlist
Show Playlist
Hide Playlist
Bronchitis and Pneumonia: Summary
-
Slides 01 URTIBronchitisPneumonia RespiratoryAdvanced.pdf
-
Download Lecture Overview
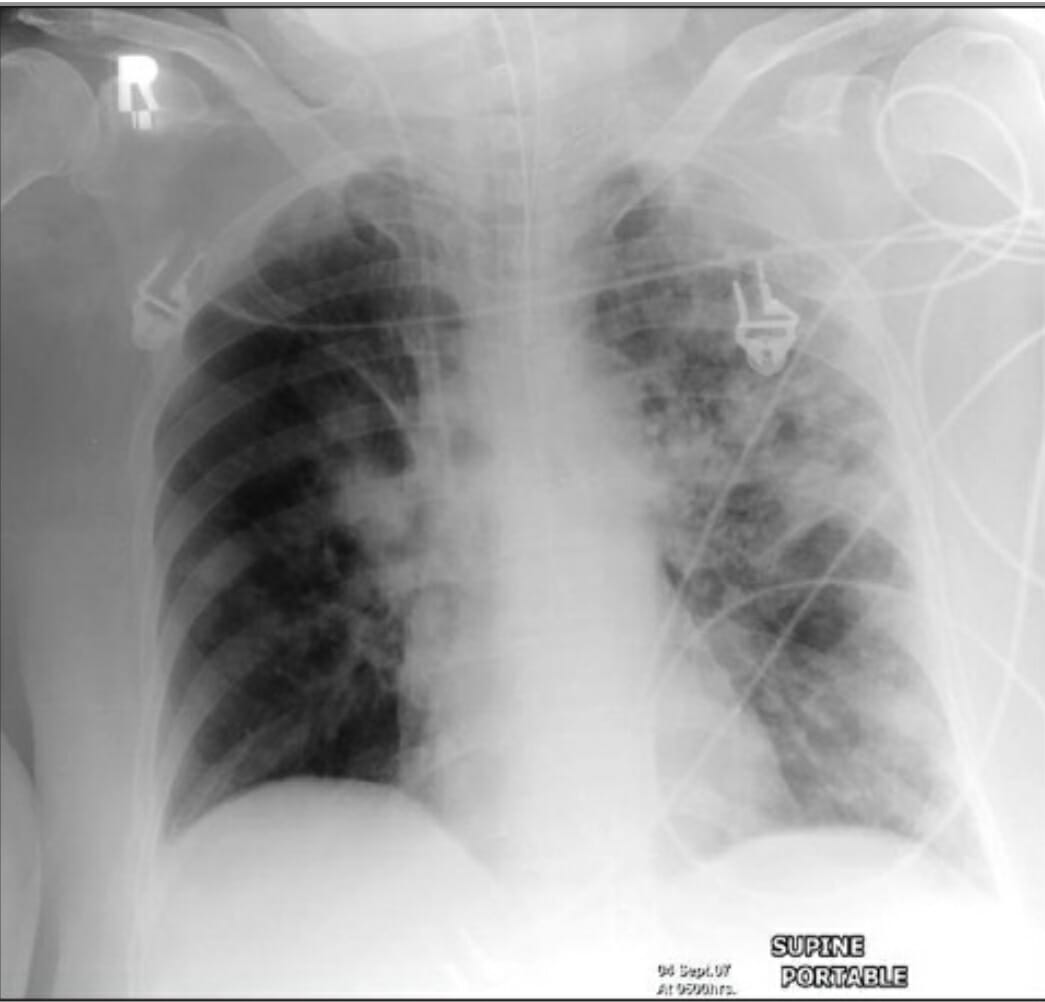
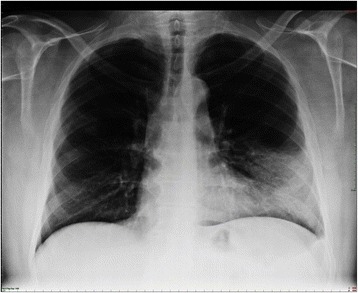
00:00 So just to summarize the main learning points of this lecture, lung infections are terribly common, and they are defined by the anatomical site, upper respiratory tract infections, lower respiratory tract infections divided into trachea and bronchial infections, tracheobronchitis or a pneumonia and alveolar infection. 00:20 So if you have infection, evidence of an infection, plus evidence of consolidation, clinically crackles, chest-ray findings with consolidation visible in chest X ray that means the patient has pneumonia. And pneumonia is classified according to where the patient is when they develop it and their background state. So community acquired which is the dominant one, the most important one, then there is the hospital acquired, ventilator acquired that we discussed, the diseases acquired whilst you're in the hospital, and pneumonia affecting immonocompromised patients, severely immunocompromised patients. And because these different types of pneumonia have different microbial causes, they require a different antibiotic regimens. 01:00 The important thing here is the common causes of community acquired pneumonia is pneumococcus, mycoplasma, chlamydia, and influenza, and whatever agent you use to treat patients, you need to cover those bacteria. So how do we manage patient with community acquired pneumonia? We assess the severity using the Curb65 score plus clinical judgment just to make sure we are not missing people whose Curb65 score is low for some reason but actually are severely unwell. Investigations, we need to confirm the presence of consolidation using a chest X ray, we need to assess how severe the hypoxia might be using blood gases, and we can try and identify the infecting organisms using blood sputum cultures and urine antigen tests that we discussed earlier. Treatment is very simple oxygen, oxygen, oxygen. 01:44 You must correct the oxygen level plus antibiotics. 01:48 Intravenous fluid replacement is important to correct the dehydration and the potential chance of hypotension and acute kidney injury. And you need to work out whether the patient is responding to therapy and that requires monitoring the temperature, the respiratory rate, the oxygen saturations, and it can be reinforced by remeasuring the C-reactive protein level which should fall as the inflammation settles and the patient improves. Thank you for listening.
About the Lecture
The lecture Bronchitis and Pneumonia: Summary by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Infections of the Respiratory Tract.
Included Quiz Questions
A 67-year-old man presents to hospital with pneumonia. Which of the following is NOT a likely cause of a persistently elevated CRP above 100 after day 5?
- Development of a deep vein thrombosis
- Development of a complex parapneumonic effusion
- Intravenous cannula site infection
- Development of a lung abscess
Which organism has a much lower incidence in immunocompromised patients compared to patients with community-acquired pneumonia?
- Streptococcus pneumoniae
- Pseudomonas aeruginosa
- Aspergillus fumigatus
- Cytomegalovirus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good Lecturer, professional appearance, good selection of high yield topics, combined with simple but important explanations on key physiopathological issues. Great experience.