Playlist
Show Playlist
Hide Playlist
Brain Death, Decorticate Posturing, Persistent Vegetative State and Locked-In Syndrome
-
Slides 10 AlteredMentalStatusandComa Neuropathology II.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
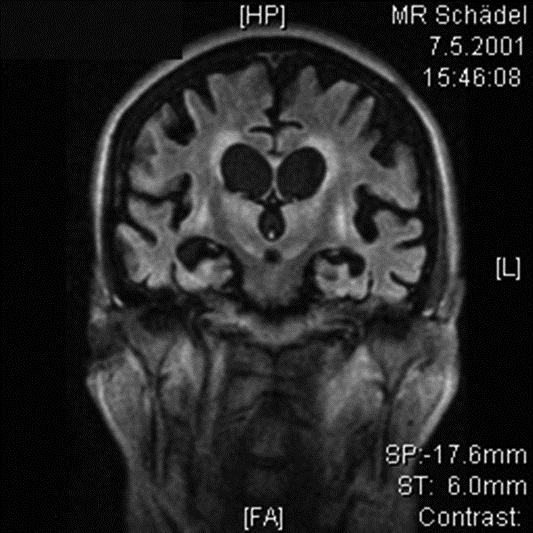
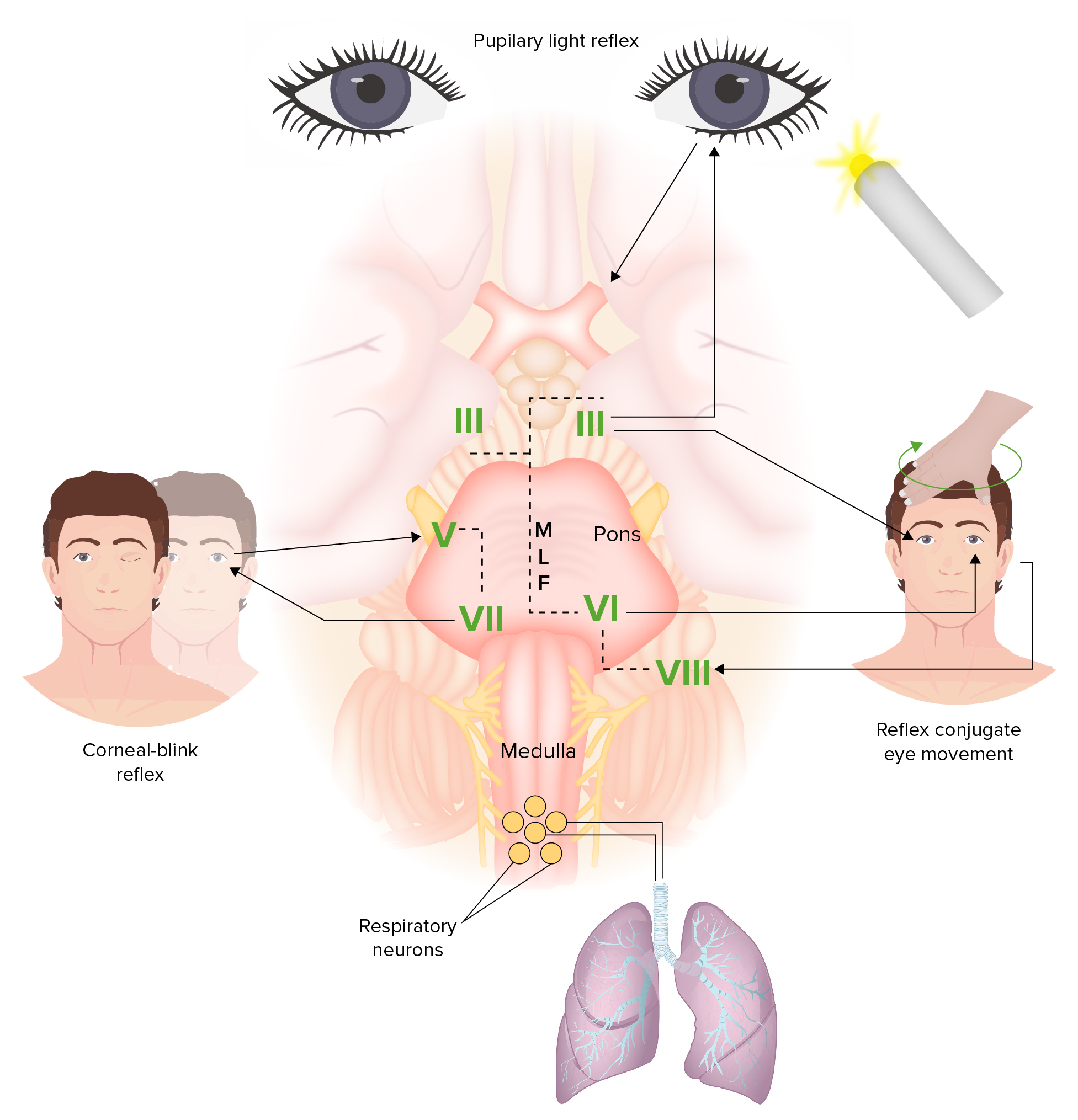
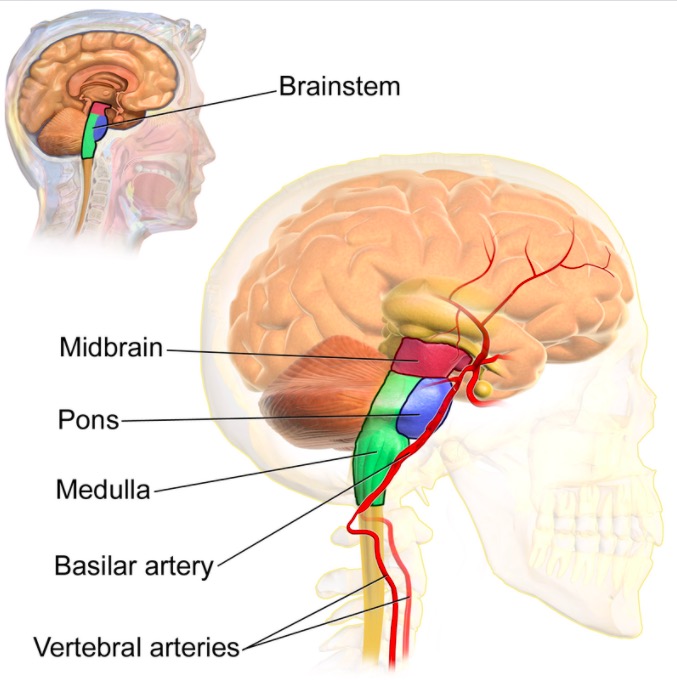
00:01 Brain death, irreversible cessation of brain and brainstem functioning, regardless of cause. 00:08 Requirements varies from, well, state to state, hospital to hospital. 00:13 Comatose, absence of brainstem reflexes that we talked about. 00:17 No spontaneous respiration. 00:21 Absence of complicating factors: Hypothermia, sedatives, metabolic abnormalities. 00:30 Approach to brain death. 00:32 Here, we have an algorithm or flow chart. 00:35 And from the flow chart, on the top, we go from the coma. 00:38 Is it present? And if it is, your next step of management is going to be neuroimaging and maybe CSF evaluation, as long as intracranial pressure is not elevated. 00:50 If you find something to be interesting, yes, then you want to start thinking about how to rule things out. 00:56 Was it hypothermia? Was it intoxication? Was it sedatives? Or was it neuromuscular blocking type of agents? Was it metabolic in terms of severe electrolyte disturbances? Was it acid-based disturbance? Or was it endocrine type of crises such as Addison’s disease? So here, what we mean by this is the brainstem reflex such as a pupillary or the cold caloric or the doll’s eye, whatnot. 01:19 Then you should perform an apnea test. This has the following steps: First ensure your patient is hemodynamically stable. Then adjust your ventilator settings to normocarbia, so that the partial pressure of C O 2 should be 35 to 45 millimeters of mercury. With this setting discontinue ventilator for 8 minutes. In brainstem death there are no spontaneous respirations. 01:44 That’s what we call apnea - despite the hypercapnia. Also obtain an arterial blood gas at 8 minutes and then reconnect the ventilator. The partial pressure of carbon dioxide is expected to be 60 millimeters of mercury or more, or 20 m m H g above the baseline value. 02:02 Next, what would you do? Clinical diagnosis of brain death is what you’re thinking. 02:09 At this point, maybe, maybe, there is eligible for organ type of harvesting, because now at this point, you’re thinking about asking the family members or a power-of-attorney as to whether or not the harvesting of organ from your patient is your next step of management. 02:27 As objective and as cold-hearted as it may seem right now, please make sure that you’re very objective on your boards and your wards. 02:37 So, your patient here, even though you wish to be optimistic at some point, you must know what your next approach would be. 02:46 Now, if the patient, no for harvesting, at this point, you get into disconnection or the ventilator becomes the question or the point of concern. 02:59 Disconnect your ventilator. 03:02 If yes, then you proceed with the donor procurement. 03:05 Here’s a brief little overview of what you can expect from going from coma to brain death to your ventilator. 03:13 Here, we’ll talk about the different types of posturing. 03:17 And by this, I mean either decorticate or decerebrate. 03:21 We talked about that Glasgow coma scaling. 03:25 And now at this point, you were thinking about level of consciousness and whether or not your patient was even awake. 03:30 As you move from six to one, at that point, I had pointed out to you different types of posturing that may occur as you lose more and more of your awakening. 03:42 Here, we have decorticate. 03:45 Would you please take a look at your patient? This is important. 03:48 What I want you to do immediately is I want you to focus upon the elbows, and I want you to focus upon the ankles. 03:56 You’ll notice here, please, that the elbows are flexed and the wrists are flexed in very tight posture, almost as if like you’re jumping out of a plane into the sea where you are just being aerodynamically efficient. 04:13 And take a look at the toes, we have plantar flexion,, and all of this is then representing the posture that you can expect with decorticate. 04:20 I need you to spend a little bit of time to make sure that you have firmly implanted the image of decorticate and its posture in your head. 04:30 So, bilateral flexion at the elbows and wrists. 04:34 Extension of the lower extremities. 04:36 We have poor localizing value. 04:39 Indicates a lesion. 04:40 Where? One of the most important points on this slide is this. 04:45 With decorticate, indicates a lesion above the red nucleus, above the red nucleus, above the red nucleus. 04:56 Less ominous that of, what we’ll get into next, known as your decerebrate posturing. 05:03 So, if this is above the red nucleus with decorticate, then decerebrate must be below the red nucleus where we have possible injury. 05:14 Please take a look at decerebrate posturing. 05:18 With decerebrate posturing versus decorticate, here immediately, I want you to jump to the elbows and the wrists. 05:27 At this time, we find that the elbows are extended. 05:31 And we also have the wrists that are extended. 05:34 Completely opposite that of decorticate. 05:38 The extension of lower extremity would be similar in both. 05:41 And most typically, indicates a lesion. 05:43 Where? Below the red nucleus and maybe, perhaps, the mid brain. 05:47 Once again, below the red nucleus with decerebrate. 05:52 Rarely seen in severe cases of toxic or metabolic encephalopathy. 05:58 Be familiar with the posturing. 06:00 One is called decorticate, the other one is called decerebrate. 06:04 So, what does a vegetative state mean to you? A vegetative state may develop after prolonged coma with continued life support. 06:13 Patients maintain respiration and autonomic functioning. 06:17 Eye opens and may blink to threat and exhibits sleep-wake cycles. 06:23 No awareness or interaction with the environment though with the vegetative state. 06:27 Prolonged coma. 06:30 Something called locked-in syndrome. 06:32 Where is this occurring? You should be thinking pons immediately, most often due to hemorrhage. 06:38 Patients unable to move extremity. 06:40 Literally, they are locked in, unable to move extremity or face, unable to vocalize, they’re trapped in their own body. 06:48 Extremely frustrating if you can imagine. 06:50 Completely awake and often cognitively intact with careful testing. 06:56 Can communicate with vertical eye movement and blinks, and that’s important. 07:01 So, then you get into habit of communicating with your patient virtually with the eyes.
About the Lecture
The lecture Brain Death, Decorticate Posturing, Persistent Vegetative State and Locked-In Syndrome by Carlo Raj, MD is from the course Altered Mental Status and Coma. It contains the following chapters:
- Brain Death
- Decorticate Posturing
- Persistent Vegetative State & Locked-In Syndrome
Included Quiz Questions
What PaCO2 level indicates a positive apnea test?
- > 60 mm Hg
- > 50 mm Hg
- > 16 mm Hg
- > 66 mm Hg
- > 40 mm Hg
Where is the site of the lesion in decorticate rigidity?
- Above the red nucleus
- Below the red nucleus
- Midbrain
- Pons
- Medulla
A large pontine lesion may result in what condition?
- Locked-in syndrome
- Persistent vegetative state
- Coma
- Decerebrate rigidity
- Decorticate rigidity
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |