Playlist
Show Playlist
Hide Playlist
Bradyarrhythmias: Management
-
Emergency Medicine Bradycardia.pdf
-
Download Lecture Overview
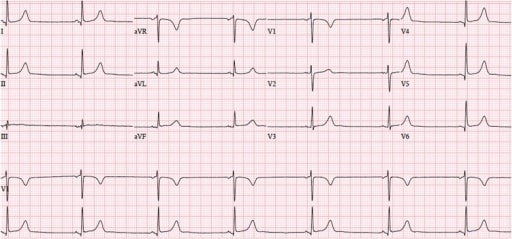
00:01 So the first line treatment for symptomatic or unstable bradycardia is gonna be atropine which is a parasympathetic antagonist. 00:10 Now we talked about how one of the causes of bradycardia is high parasympathetic tone. 00:14 So you can imagine blocking the parasympathetic input to the heart is potentially gonna speed the heart back up. 00:20 The dose is generally gonna be half a milligram given every three to five minutes You can give a max of three milligrams before your patient is maximally atropinized, and there’s not gonna be any additional benefit. 00:33 You also can use infusions of sympathomimetic so dopamine or epinephrine can be used to raise the sympathetic tone, it’s given as a continuous infusion and titrated to the desired blood pressure and heart rate parameters. 00:49 But you wanna be really careful with these if you think ischemia is the underlying cause for your patient because both dopamine and epinephrine increase myocardial oxygen demand and can exacerbate ischemia. 01:02 So these should be really used with caution. 01:06 More typically if we have a patient who has symptomatic bradycardia, we’re gonna move to pacemaking rather than medical management. 01:14 So transcutaneous pacing is the immediate first line pacemaking approach that we used in the emergency department because it can be completed very quickly. 01:24 So you accomplish this by putting external electrodes or pacer pads on the patient and you can see the location on the diagram where those go on the body. 01:32 You always wanna make sure your patient has oxygen, they’re on a cardiac monitor and they have adequate IV access before you initiate pacing. 01:41 And when possible you wanna sedate your patient. 01:44 Now, if they're too unstable to do that, and you need to initiate pacing immediately, you can for go sedation. 01:51 But generally you know, you’re actually shocking the patient repeatedly when you pace them and it’s quite uncomfortable for them, so you wanna provide sedation whenever it’s feasible to do so. 02:02 The way you initiate transcutaneous pacing is actually pretty straight forward. 02:07 So you’re gonna sat your defibrillator to the pacer setting. 02:10 You’re gonna set a heart rate of 80 to a hundred. 02:13 So you wanna make sure that heart rate is significantly higher than the patient’s current heart rate, so that you’ll be able to tell when you get pacer capture. 02:22 You’re gonna start off with the low amperage, a low amount of energy, and you’re gonna gradually dial it up until you get capture. 02:29 Meaning each pacer's spike produces QRS complex. 02:33 Once you get captured, you gonna go up by ten milleamperes. 02:39 And that’s where you’re gonna stay for the whole time your transcutaneously pacing. 02:45 And again, once you have pacing established, you definitely wanna provide sedation and that sedation should be continual until such time as you terminate transcutaneous pacing. 02:55 Because this is actually physically shocking the patient repeatedly, 80 to a hundred times per minute, and it’s quite uncomfortable for a conscious person. 03:04 Now, your more definitive alternative is transvenous pacing. 03:10 And this is something that's a little bit more complex to do, it definitely requires specific training, and it’s not something you would wanna do in the emergency setting if you haven’t specifically learn how to do it. 03:23 But basically the way the procedure works, is you introduce a central venous catheter that’s large in caliber, it's a sheath that will let you put pacer wires through it. 03:32 Your two options for catheter insertion are the right internal jugular which is marked here, or the left subclavian vein. 03:41 What you're gonna do once you have your sheath in place, is you’re gonna put electrodes through the sheath, and advance them through the venous system into the apex of the right ventricle which is marked right there on the diagram. 03:54 You have an external control panel that allows you to control the heart rate and the amperage. 04:01 And the nice thing about this, is that it’s painless for the patient. 04:04 I mean obviously introducing the sheath initially can cause some pain. 04:09 But once you have the sheath in place and you have the electrodes inserted, the patient can’t feel this, the way they can feel transcutaneous pacing. 04:17 So you don’t need to provide any ongoing sedation. 04:20 It’s also a much more reliable than transcutaneous pacing. 04:23 So you basically have an electrode that’s in physical contact with myocardium and it’s pretty easy to get pacer capture, and to initiate cardiac contraction with each pacer impulse. 04:37 So bottom-line, is that fortunately the vast majority of bradycardias are not emergencies and emergency treatment is only necessary for unstable patients. 04:47 Now in the long term, some stable patients might require treatment but in the ED setting, we’re only gonna be addressing bradycardia, if the patient is unstable. 04:57 You can use the EKG to differentiate between different bradycardia types, and it’s very important that you do so because the different bradycardias have different pathophysiology and different prognoses. 05:10 So you wanna make sure you know what rhythm you’re dealing with, so you manage it appropriately.
About the Lecture
The lecture Bradyarrhythmias: Management by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock.
Included Quiz Questions
What is the first-line treatment for symptomatic bradycardia?
- Atropine
- Adenosine
- Amiodarone
- Epinephrine
- Labetalol
What is the maximum dosage of atropine given to treat a bradycardic patient?
- 3 mg
- 1 mg
- 1.5 mg
- 2 mg
- 2.5 mg
Which of the following statements about transcutaneous pacing is TRUE?
- Sedation is recommended to avoid discomfort due to repeated electric shocks.
- It is introduced via a central venous sheath.
- It provides a more reliable capture compared to transvenous pacing.
- It requires specific training.
- Four electrodes are placed directly on the apex of the right ventricle.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank you, it was very well explained. Going through these videos fast.