Playlist
Show Playlist
Hide Playlist
Bone Marrow Failure (BMF)
-
Slides Normocytic Non-Hemolytic Anemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
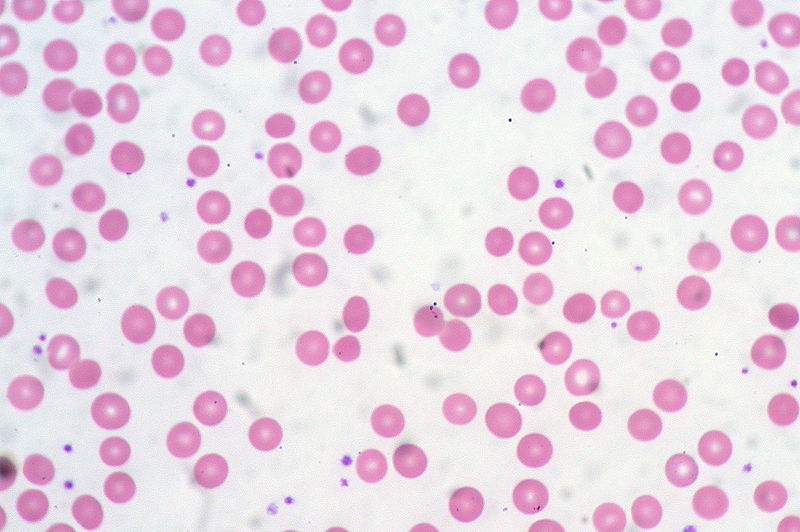
00:00 Now moving forward, apart from acute blood loss and still in the realm of normocytic non-hemolytic anemia, let us now move in to the bone marrow and for whatever reason we're going to shut it down. If you shut down your bone marrow, then what happens? Well, you can't produce reticulocytes. Can you? So therefore what's the concept? It's the fact that you have a decreased reticulocyte production index or, as it says here, inadequate reticulocytosis and that magic corrected reticulocyte number is less than 3%. That you'll have to memorize but the concept is clear. It's the fact that the bone marrow has been shut down. Why? Well, we'll get in to this in a second. Bone marrow cellularity, rule of thumb. So if the bone marrow has been shut down, think about what the bone marrow should look like. It should be nice and empty. There should be lipid, there should be fat vacuoles, and obviously there should be hematopoietic stem cells and there should be those primitive fibroblasts. Right? Not too much and not too little, just right and so that you can then produce a proper homeostatic churning or synthesis of the stem cells that we require. However, if the bone marrow, for whatever reason let's say that this patient has aplastic anemia, then understand that at this point the bone marrow is completely dead end and it's pretty empty. I'll show you pictures. Now, as a rule of thumb, what you can use is 100 minus age gives you approximate normal cellularity of your bone marrow. Alright, just generality but as far as you're concerned it would work. Pancytopenia is just the term that we use for what please, usually it's in reference to the trilineage and by trilineage we're referring to obviously the RBCs, the platelets. And of all the granulocytes which one do we normally have in our body circulating predominantly? Good. Neutrophils. So that's usually what you're referring to when you say pancytopenia and each one of those loss of the lineages is going to give you different symptoms in your patient. 02:06 For example, if there's no RBC your patient is going to present how, fatigued and tired. 02:12 If your patient has not enough platelets, what is that presenting with? Obviously excess bleeding, they can form a clot. And if they don't have neutrophils then what does that mean to you? Oh, they're now susceptible to infection. There is the 3 that you want to take a look at when you have pancytopenia. Earlier, we talked about this in terms of megaloblastic anemia. Right? In megaloblastic anemia, remember please, you are still producing your cells but they were blasts but just because you form a cell if it hasn't matured then it can't carry out its function. Can it? Of course not. So there's a megaloblastic anemia or the megaloblastic cells and hypersegmented neutrophils with B12 and folate. Yes there is pancytopenia but that is not aplastic anemia. Is that clear? By definition, if it's aplastic anemia, it means that you had no cells being produced because the bone marrow had been shut down and so therefore you're in the category of normocytic, non-hemolytic anemia. Keep that in mind as you move forward. Now, bone marrow failure, idiopathic autoimmune being the most common. You'll find that occurring with many organ damage. Drugs including chloramphenicol and chemotherapy, chemo suppression right in general or bone marrow suppression usually looking at those cells that like to divide. Tell me about your stem cells. What kind of cells are they? They're labile. Aren't they? They love to proliferate, proliferate, proliferate and so therefore with chemotherapy looking at those cells that love to proliferate and unfortunately instead of attacking the cancer may also have collateral damage. 03:49 You've heard of bone marrow suppression, you've heard of hair loss, and there is massive diarrhea. Isn't there? And those patients that are taking chemotherapy unfortunately, quite a bit of pain. Sometimes the chemo is worse than the disease itself, uhh. Infection. We have parvovirus B19. Now, what we'll do here is well. 04:06 Is anytime parvovirus is it possible that you might have a patient that has another type of anemia such as hemolytic anemia and they may then have a parvovirus B19 virus infection. Sure. And so therefore at that point we already moved in to, what's my topic here or category? Normocytic non-hemolytic because the bone marrow has been shut down. Now, with Diamond-Blackfan syndrome, we'll talk about this a little bit more, but what I do wish for you to keep in mind is the following. 04:36 Diamond-Blackfan syndrome can come under either your bone marrow failure where this is normocytic, non-hemolytic, and please be very careful because Diamond-Blackfan could also be part of your megaloblastic anemia. We'll talk more about that later but that's one that you want to pay attention to. Fanconi's anemia there. What you want to pay attention to is do not confuse that with Fanconi syndrome. Which is a problem with the proximal convoluted tubule in the kidney, one has nothing to do with the other. These are all the different causes that you want to be quite familiar with with bone marrow failure.
About the Lecture
The lecture Bone Marrow Failure (BMF) by Carlo Raj, MD is from the course Normocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following is NOT a feature of aplastic anemia?
- Hypercoagulable state
- Fatigue
- Bleeding diathesis
- Increased risk of infections
- Decreased reticulocytosis
Which of the following does NOT result in aplastic anemia?
- Decreased DNA synthesis
- Chemotherapy
- Bone marrow suppression
- Fanconi anemia
- Parvovirus B19 infection
Which of the following could present as megaloblastic or normocytic anemia?
- Diamond-Blackfan anemia
- Iron-deficiency anemia
- Sideroblastic anemia
- Anemia of chronic disease
- Thalassemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |