Playlist
Show Playlist
Hide Playlist
Anticoagulants and Plaque – Cardiovascular Pharmacology
-
Slides 06 Cardiology Alpert.pdf
-
Reference List Introduction to the Cardiac System.pdf
-
Download Lecture Overview
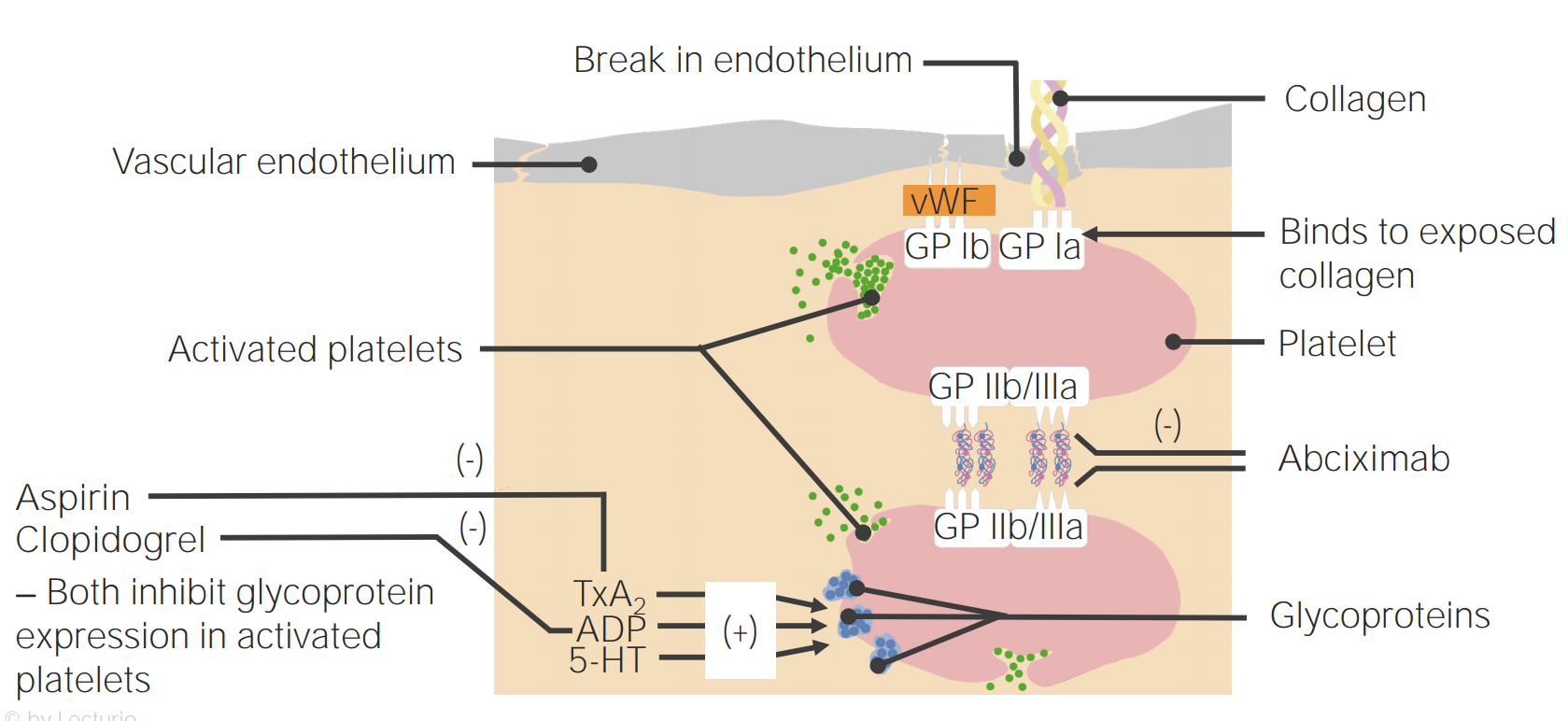
00:00 Now, let’s move now from the Statin drugs, let’s talk about anti-coagulants. As you probably already are aware, many of the cardiovascular events that occur with atherosclerosis are the result of blood clots that form over the atherosclerotic lesions. When a blood clot forms in the heart, it causes a myocardial infarct or heart attack. When a blood clot forms in the arteries to the brain, it causes a stroke. And so, one part of the treatment of these diseases is an attempt to dissolve the blood clots and a second part is to keep the blood clots from forming. We have a variety of drugs that block the clotting system. The first group are known as anti-thrombotics. They are very powerful anti-coagulants. At least one of them - heparin, can be given intravenously. Many of them can be given as subcutaneous injections and some can be given as oral agents. That’s the second category on this slide, the oral anti-thrombotics. The oral anti-thrombotics have a similar very powerful anti-coagulant or blood thinning effect, often as powerful, for example, as heparin. The commonly used one is warfarin. Warfarin blocks a number of the clotting factors in the clotting cascade - factors II, VII, IX and X. It’s a very, very effective anti-coagulant. 01:35 And then there are some new agents, factor X blockers and factor II blockers that, in many ways, are a little more effective than warfarin because they are little more easily you thin the blood… what’s the risk for the major side effect? Bleeding. And sometimes, you thin the blood… what’s the risk for the major side effect? Bleeding. And sometimes, that bleeding can be fatal. So, we cardiologists, we would like to use these drugs, but we use them very, very carefully. I always think of them just like firearms, just like guns. 02:10 They are useful under some circumstances, but you have to be very careful with them and you have to know what you are doing when you use them. 02:17 So, when do we use heparin or two of the others, fondaparinux or argatroban? We usually use intravenous heparin in the earliest or acute phase of a heart attack. When we have done something to remove the blood clot, either with drugs, thrombolytic drugs or with angioplasty - the little balloon catheters and stents that are used to open up the artery and pull the blood clot that’s formed in the artery out. And what we do is we put patients on heparin the injury to the heart muscle all over again. Once we are finished with our short course the injury to the heart muscle all over again. Once we are finished with our short course of heparin, usually and often in these patients, a stent has been placed - the little wire cage. 03:02 We are going to talk a lot more about that when we talk about coronary artery disease later in this series. We then put the patients on anti-platelet agents. 03:10 Platelets are the first step in the clotting cascade. So, when you cut yourself, what happens is, eventually a little blood clot forms and a little scab forms, right? Well, the first step in that is activation of little bodies that float throughout the bloodstream called platelets. When they see an injury like that, they become activated. They release a number of chemicals that then start a whole series of chemical reactions that end up in the blood clot. So, why do we put people on anti-platelet agents? It’s to prevent blood clots from forming both on top of a new stent or even chronically in somebody who already has atherosclerotic coronary artery disease. Interestingly enough, the commonest anti-platelet agent is aspirin. You may have noticed if you cut… if you have taken some aspirin, let’s say for a headache and you cut yourself, it takes you a much longer time to stop bleeding once you are on aspirin. 04:06 The commonly used ones are clopidogrel, prasugrel and ticagrelor and these have been approved in the United States and also in Europe. They are used after stents and… and various procedures in the coronary arteries have been done. They are used long term in people who are at high risk for forming blood clots. The oral anti-coagulants are used to prevent clots that can form inside the heart, particularly with an arrhythmia known as atrial fibrillation. 04:35 In a few moments, I am going to talk about that some more, but atrial fibrillation is an irregular heart beat in which the atria of the heart, instead of beating nice and regularly like this, fibrillate, they quiver. And in that quivering state, blood clots can form within the left atrium. They can get out of the left atrium into the circulation and go to the brain and cause strokes, go to the kidney and cause kidney damage and so forth. So, a lot of bad things can happen with the blood clots when they form in atrial fibrillation. And it’s been shown that with blood thinners, with anti-coagulants, oral anti-coagulants, we can markedly decrease the risk for these blood clots forming in the heart and getting out. Warfarin has been the gold standard for a long time. It’s a drug that’s… that is much more complicated to deal with than some of the newer agents. It requires constant blood tests, it requires changes in diet and it is associated with more bleeding, particularly bleeding in the brain, which is as you can imagine the worst possible place to bleed. And that’s why new agents have been developed. 05:39 The factor Xa blockers, there are now three of them approved in the United States - rivaroxaban, apixaban and edoxaban. And then there’s a factor II blocker, only one there, that’s dabigatran. And each of these agents are approximately equal in efficacy. They are just as good as or maybe a little better than warfarin and they are associated with a little less brain bleeding. Well, let’s talk a little bit about the atherosclerotic process itself. We are going to come back to talk about this again, but remember that inflammation is the factor that starts the whole injury in the arteries that then leads downstream to atherosclerosis. It’s felt that what happens is the endothelium which is the small skin on… lining the arteries is injured by a variety of things. Maybe a viral infection, maybe cigarette toxins - toxic things that are in cigarette smoke, maybe then more permeable to substances in the blood. Guess what... which one gets in? Cholesterol. 06:41 then more permeable to substances in the blood. Guess what... which one gets in? Cholesterol. 06:49 When cholesterol gets in onto the endothelium, it sets off an inflammatory reaction. Just like a mosquito bite, for example, is an inflammatory reaction. Inflammatory cells and inflammatory chemicals are released by the body, that’s what makes it itch and you scratch at it. 07:02 Well, of course, you can’t scratch the inside of your coronary artery, but the same inflammation process starts there and unfortunately, cholesterol is a very potent stimulus for inflammation. 07:16 And once it gets started, it doesn’t stop. And consequently, once it keeps going, more cholesterol is able to get in there. There’s more inflammation. Eventually, you end up with an atherosclerotic plaque. These can be very large or they can be small. Sometimes the small ones are very friable or very tender and they can break and suddenly, that sets off the clotting cascade and a blood clot forms and the artery is blocked. 07:43 Now, here is an anatomical picture from somebody who died, not from a heart attack, but from something else. But you can see, it’s a cross section of a coronary artery and you can see at the bottom there, there is a little collection, sort of looks like a cottage cheese. 08:04 That’s cholesterol in a large atherosclerotic plaque. 08:08 The good news is in this patient, you can see that the channel, which is the black area, is still open. So, there’s plenty of blood flow going down there, but what can happen is, the little cap - the little endothelial cap that’s covering that cholesterol can crack or break exposing the bloodstream to the underlying cholesterol and a blood clot can form and here we see an example. You can see that there has been a little bit of the endothelium peeled off into the lumen, and that black substance is not an open channel. 08:41 It’s a blood clot in this patient who had a fatal myocardial infarction, a fatal heart attack from the blockage of the artery by the blood clot. 08:52 Now, as we talked about before, when a patient has a myocardial infarct or often when they have a stroke and we get rid of the blood clot, either mechanically or with drugs, we then put the patient on heparin for a while. We can give that intravenously and for a few days or it can be given subcutaneously with injections. Usually, for myocardial infarction, we don’t put patients on the long term chronic agents like warfarin or the newer agents I talked about - rivaroxaban, apixaban and edoxaban. Why not? Because the data has not shown that long term treatment with those agents prevents a second heart attack. 09:35 In fact, it turns out that the data from the randomized controlled… double-blind controlled trials show that the anti-platelet agents are more effective. It is true that the anti-coagulants like warfarin and rivaroxaban and so forth do prevent blood clots, but they increase agents have much less problem with bleeding. And so, therefore, even though they are not agents have much less problem with bleeding. And so, therefore, even though they are not quite as effective at decreasing clots, they are much safer. So, you end up with a positive benefit in the end using the anti-platelet agents. And they are all so much easier to use, of course, because they can be taken as pills. 10:15 Now, let’s talk then about evidence based medicine in other things for… other aspects of evidenced based medicine for the patient with coronary artery disease or strokes. 10:27 First of all, we have already of course, talked about the Statins. We also usually put these patients on aspirin. If they have had a stent placed or a procedure done in their coronary arteries, even coronary bypass, they may end up on a double program of anti-platelet agents. that is aspirin plus clopidogrel or one of the newer anti-platelet agents - prasugrel or ticagrelor. Stroke patients sometimes end up on aspirin and dipyridamole, that’s another combination that works as anti-platelet. And the newest agents - prasugrel and ticagrelor are slightly more effective than the older agent clopidogrel when combined with aspirin, but maybe associated with more bleeding. And that’s not a surprise, of course, because the more effective any anti-coagulant is, the more likely you are to see bleeding complications.
About the Lecture
The lecture Anticoagulants and Plaque – Cardiovascular Pharmacology by Joseph Alpert, MD is from the course Introduction to the Cardiac System.
Included Quiz Questions
Which of the following medications is considered an antiplatelet agent?
- Clopidogrel
- Argatroban
- Heparin
- Warfarin
- Fondaparinux
Which of the following medications are preferred for stroke prevention in patients with atrial fibrillation?
- Blockers of factors Xa or IIa
- Warfarin
- Aspirin
- Fondaparinux
- Argatroban
Intravenous heparin would be best used in which of the following situations?
- In a patient with myocardial infarction which was treated by coronary angioplasty
- In a patient with stable angina
- In a patient with atrial fibrillation
- In a patient with a recent epidural hemorrhage
- In a patient with carotid artery stenosis
Which of the following events is considered the first step in atherosclerotic plaque formation?
- Endothelium injury
- Cholesterol sequestration
- Macrophages activation
- Rupture of the fibrous cap
- Smooth muscle cells migration
Warfarin exerts its anticoagulant effect through which of the following mechanisms?
- Inhibition of the production of the clotting factors II, VII, IX, X
- Activation of antithrombin 3
- Inhibition of platelet activation
- Acting as a vasodilator
- Direct inhibition of factor Xa
Which of the following pairs is matched correctly?
- Apixaban/atrial fibrillation
- Heparin/oral anticoagulant
- Warfarin/parenteral anticoagulant
- Aspirin/clotting factor production inhibition
- Direct thrombin inhibition/heparin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
2 customer reviews without text
2 user review without text