Playlist
Show Playlist
Hide Playlist
Anomalies of the Aging Brain: Dementia (Alzheimer's Disease)
-
Slides 02 AnomaliesAgingBrainAlzeheimerDementia Aging.pdf
-
Download Lecture Overview
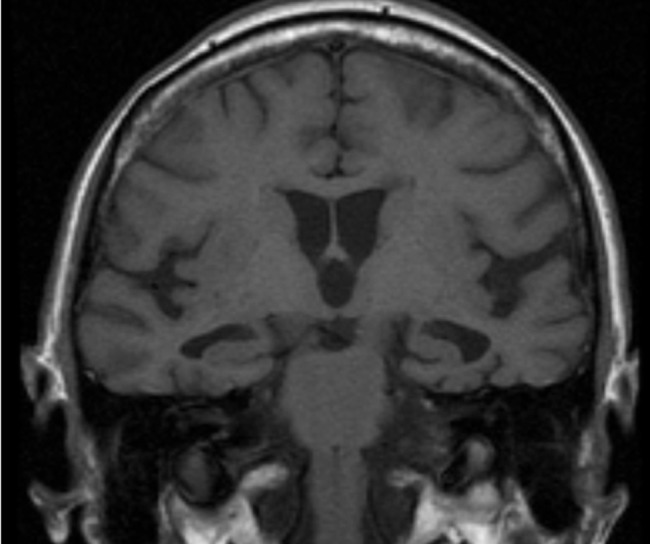
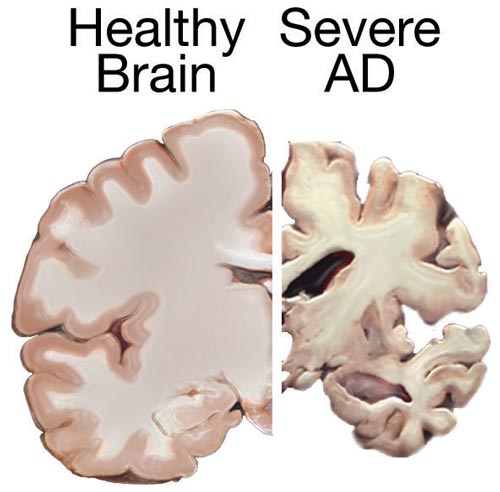
00:01 This is the first of two lectures on anomalies of the aging brain. In this lecture, we’ll be discussing dementias as well as delirium. We’ve all had the experience of walking in to the other room and wondering what did I ever come in here for. It’s natural that that sort of pattern will increase slightly with age. Normal forgetfulness is normal forgetfulness. It doesn’t really cause too many deep-rooted problems. However, if that sort of thing progresses to a decline in reasoning and judgement as well as memory, so we see progressive loss beyond the usual, we see that there is development of dementia. There are a number of different kinds of dementia. 01:00 Dementias are most common in individuals over 65 years old. So, there’s normal memory loss and then there’s excessive memory loss which might involve loss of reasoning and judgement. 01:14 People start to seem a little bit loopy. Anyway, Alzheimer’s is probably the one that you’d think of most clearly when you think about dementia. That’s probably because about 60% of dementias are accounted for by Alzheimer’s. Alzheimer’s, you’re probably familiar is a neurodegenerative disorder. 01:38 It has some hereditary association but we haven’t quite deciphered the multifactorial pieces associated with that. What we do know is that it is associated with development of plaques and tangles in the brain. At that level, you probably already understand this. 01:58 We don’t know if the tangles and plaques are a cause of the dementia or whether they result from the development of dementia. We just know that they are associated with that. So, cause or effect, that’s pretty much unclear at the moment. But let’s take a closer look at the regions of the brain that could be associated with Alzheimer’s. Generally, it’ll start in the temporal lobe. 02:27 In the temporal lobe, if that is the area associated with damage, the individual is more likely to forget things. If the damage is primarily in the frontal cortex, the individual might have trouble planning things. Really, it depends on the region of the brain that’s most affected where Alzheimer’s shows up first. It does have a classic sort of progression. 02:51 I’ll lead you through that shortly.
About the Lecture
The lecture Anomalies of the Aging Brain: Dementia (Alzheimer's Disease) by Georgina Cornwall, PhD is from the course Aging.
Included Quiz Questions
Which of the following statements regarding dementia is true?
- Dementia is a progressive decline in brain functioning.
- Dementia is part of normal brain aging.
- Dementia is a sudden decline in memory.
- Dementia is most common in patients less than 65 years old.
- Dementia is never hereditary.
Which of the following statements regarding Alzheimer's disease is correct?
- Alzheimer's disease has some hereditary associations.
- Alzheimer's disease is a muscular-degenerative disorder.
- Alzheimer's disease can be associated with plaque build-up in the frontal lobe of the brain, associated with increased forgetfulness.
- Alzheimer's disease can be associated with plaque build-up in the temporal lobe of the brain, associated with increased difficulty with planning.
- Alzheimer's disease accounts for 10% of all dementias.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
excellent i learnt many things from this lectures (Dementia is very important problem) thank you
3 customer reviews without text
3 user review without text