Playlist
Show Playlist
Hide Playlist
ANCA-associated Vasculitis
-
Slides Vasculitis.pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
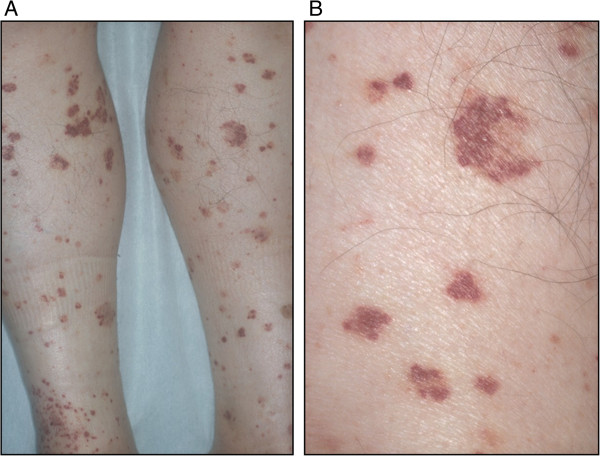
00:00 Alright, 3 more to go. Now, the ANCA-associated small vessel vasculitides, which is all the ones we've got left, they actually have a lot of things in common so let's compare and contrast them Okay, so again, this slide is going to cover all the things that are common to all of the ANCA-associated vasculitides. First off, they are called small vessel but again as I mentioned before, they do have some medium vessel involvement as well. You're going to see systemic symptoms with these diseases typically fevers, maybe weight loss, maybe malaise and there may be a prodrome of weeks to months before you start to see symptoms. In fact, with EGPA, eosinophilic granulomatosis with polyangiitis, it could be a few years before you start to see these more fulminant presentations. It may involve the kidneys and they often do, you're going to see a rapidly progressive, crescentic, pauci-immune glomerulonephritis. And on skin biopsy similar to what you saw with PAN, you're going to see subcutaneous nodules but you may see also granulomatous lesions as well. On exam, you're going to have maculo-papular erythematous rash, you may have some palpable purpura, and you may also find livedo reticularis. You're going to start to see some commonalities between all the different vasculitides and it's going to be difficult to tease them apart but we're going to do our best to get through it all. When you look at the lung exam, on chest x-ray, or on physical exam, you'll find pleural effusions, nodules, opacities, and you may also see alveolar hemorrhage but perhaps not as common as you might see it in polyarteritis nodosa. Other manifestations include the cardiovascular system where you might see heart failure or pericarditis, gastrointestinal system, again mesenteric ischemia, and also you could find mononeuritis multiplex just like we saw with PAN. With ANCA-associated vasculitides, you can have fairly quick life threatening organ involvement that will progress somewhat rapidly over time. It's actually most often the cardiac manifestations that are the most lethal manifestations of the vasculitides. In addition, you're going to find a high ESR and high CRP but these are kind of generic inflammatory markers. Now, we've had this image here on the right for all this time. We may as well talk about it. Right? So the image on the left p-ANCA, the p stands for perinuclear and that means that essentially there are anti-bodies that are surrounding the nucleus that are lighting up. It turns out that the p in perinuclear refers to myeloperoxidase as well. That's the enzyme which was later identified to be the protein that's floating around the nucleus. What's difficult to see in that slide on the bottom left is that there's a larger cell around that ring around the nucleus. So, that antibody is lighting up just around the nucleus. 02:53 In contrast, if you look at the picture on the right, c stands for cytoplasmic and that means that the protein that's being highlighted there is actually diffusely spread throughout the cytoplasm rather than being just around the nucleus and you can see the nucleus is vaguely highlighted there on the right but it's the entire cell that is being lit up. So that's what perinuclear versus cytoplasmic ANCA-associated proteins refer to. For c-ANCA, the specific protein that's highlighted is called proteinase 3. Now we have to make a very key point here. 03:25 Importantly, not all ANCA-associated vasculitis is ANCA-positive. Now that doesn't confuse you, you're not paying attention. I just said that not all ANCA-associated vasculitis is associated with a positive ANCA. I know. These are basically cases in which everything looks like a typical ANCA-associated vasculitis with a classic ANCA-associated vasculitis story, classic symptoms, classic biopsy findings but the actual serum ANCA testing is negative. Go figure. Alright, so now that we've talked about that common things about the 3 ANCA-associated vasculitides, let's talk about how to tease them apart. We'll start with GPA, granulomatosis with polyangiitis. 04:17 The characteristic feature of this one, which used to be called Wegner's, is ENT involvement; ear, nose, and throat involvement. 90% of such patients will have necrotizing lesions of the nasopharynx, this classic saddle-nose deformity which you can see here, otitis media interestingly enough, sinusitis, hemoptysis, the entire part of the ENT system can be involved here. In addition, such patients are very likely to have renal involvement and that's a crescentic glomerulonephritis, and these patients 90% of them will be c-ANCA positive and again they're staining for PR3, proteinase 3, here. In contrast, this is microscopic polyangiitis. In many ways, microscopic polyangiitis is very similar to granulomatosis with polyangiitis except, you guessed it, it doesn't have granulomas on biopsy. Otherwise, very similar presentation, similar pathology, and the other difference is it's ANCA positivity is instead on the perinuclear side with evidence of MPO staining 70% of the time. Next up is eosinophilic granulomatosis with polyangiitis which is definitely distinct from those other 2 types. This is going to have more of a pulmonary involvement type of picture rather than all that ENT involvement with the necrotizing features. These folks are going to have asthma oftentimes for a decade or more before the onset of more of the systemic symptoms. They will have some sinus symptoms. So, rhinosinusitis, nasal polyps, maybe serous otitis media but you're not going to see those destructive symptoms like the saddle-nose deformity, that sort of thing with EGPA. Most importantly, this is the most significant finding is lots of eosinophils. Whether you're going to have peripheral eosinophilia with eosinophil counts in the 10-15% range or if you perform biopsies or a broncho-alveolar lavage, you're going to find eosinophils in places you don't normally find them in great numbers. 06:16 In EGPA, in terms of it's ANCA positivity, this is one of the ones that is not always associated with a positive ANCA, in fact only about 40% of cases of EGPA will have a positive ANCA. When When it is positive, more often than not it is a p-ANCA type of picture staining for MPO. Okay, so that was all of our vasculitides that we've had in our differential diagnoses. So now that we've looked at all of them, let's look back at our patient and the diagnostic work-up that's underway. Alright, let's start to jump into our data now that we've looked at every item on our differential diagnoses. Okay, so I'm seeing right off the bat we have a little bit of an anemia with a low hemoglobin, slightly elevated white blood cell count but there is a significant finding with 13% eosinophils up there in the top right and I want that to trigger a flag, you should be thinking about EGPA as soon as you start to see peripheral eosinophilia. Creatinine of 1 is also important. That's going to really make our likelihood of having GPA, MPA, or ATGBM disease considerably less and of course the accompanying negative urinalysis supports that as well. 07:25 Those conditions usually have renal involvement. Next up, the IGE level, we hadn't talked about that before but that's one of the lab tests that can be associated with EGPA. The p-ANCA, we've talked about the different ANCA positivities here, p-ANCA is one of the ones that is more likely with EGPA, either way the fact that this person's ANCA positive should definitely take PAN off of our list. Next up, looking at the x-ray findings, yes we clearly have some pulmonary involvement, that could go for and against the couple different conditions but the big finding is the bronchoalveolar lavage, 40% eosinophils. Typically you'll only have a few percent of eosinophils present on a BAL, if any at all. So that is strongly supporting our diagnosis of EGPA. Lastly, we'll probably going to perform a skin biopsy in such a patient and in this case we would find a necrotizing vasculitis with eosinophilic infiltration and perivascular necrotizing granulomas. 08:27 This is a slam dunk for EGPA. So, have we made our diagnosis? Let's revisit some of the salient features of our H&P to just review a few things.
About the Lecture
The lecture ANCA-associated Vasculitis by Stephen Holt, MD, MS is from the course Vasculitides.
Included Quiz Questions
Which of the following biopsy findings is most consistent with granulomatosis with polyangiitis (Wegener granulomatosis)?
- Granuloma formation
- Abundant eosinophils
- Vacuolated neutrophils
- Apple-green birefringence under polarized light
- Transmural necrotizing inflammation of medium-sized arteries
Which of the following pairs is matched INCORRECTLY?
- Perinuclear antineutrophil cytoplasmic antibodies, proteinase 3
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome), chronic rhinosinusitis
- P-ANCA, microscopic polyangiitis
- Granulomatosis with polyangiitis (Wegener granulomatosis ), upper respiratory tract symptoms
- Systemic symptoms, microscopic polyangiitis
Which of the following features is NOT typically found in patients with ANCA-associated vasculitis?
- Sudden, unilateral, painless vision loss
- High erythrocyte sedimentation rate
- Purpuric rash
- Pauci-immune crescentic glomerulonephritis
- Fever
All of the following clinical features are associated with granulomatosis with polyangiitis (Wegener granulomatosis) EXCEPT...?
- ...recurrent wheezing.
- ...saddle nose deformity.
- ...fever.
- ...hemoptysis.
- ...hematuria.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is very well done. I love how he works through the differentials and shows exactly how to rule things in and out especially with real vignettes/labs. It's a lot more helpful to show it in terms of symptoms and real labs values.