Playlist
Show Playlist
Hide Playlist
Algorithm of Acute Renal Injury
-
Slides Renal AKI.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
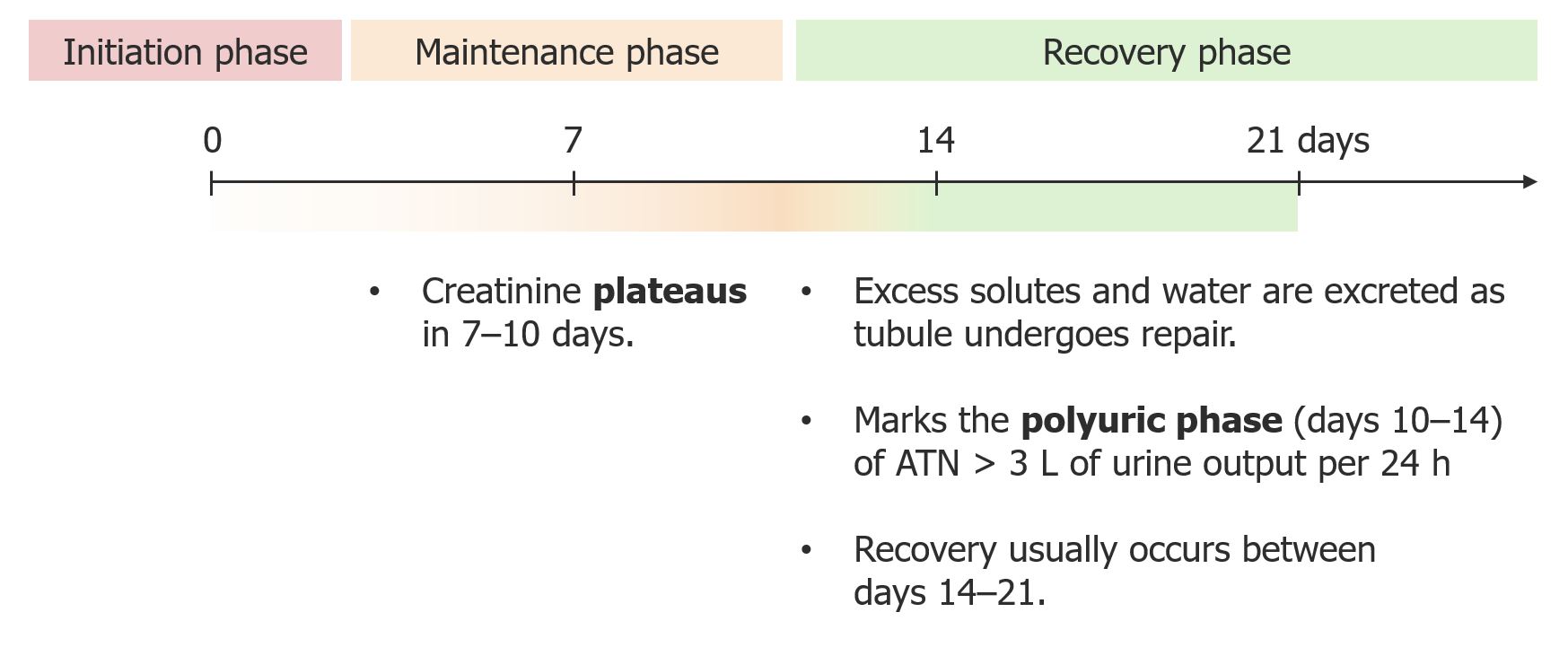
00:01 Hello and welcome to the general approach to a patient with acute kidney injury. 00:05 Today we'll be discussing an algorithm of acute kidney injury, which really builds off our kidney lecture so when our patient is sitting here before us, how do we approach them? And we think that they may have an acute kidney injury. 00:17 One of the first things that we really have to ask ourselves is, does this patient satisfy one of the kidney disease improving global outcomes or CODIGO criteria for diagnosing acute kidney injury? This includes an increase in serum creatinine. 00:30 So believe it or not, an increase of just 0.3 milligrams per deciliter or more within a 40 hour period of time is suggestive of AKI, as well as greater than 50% increase in serum creatinine within seven days. 00:43 So looking at serum creatinine, it's very important and knowing the time course of which the patient is at risk. 00:48 Now, we also want to look at urine output and having an acute decrease in urine output of greater than 0.5 milliliters per kilogram per hour for greater than 6 hours is also suggestive of A.I. 00:59 So it's important for us to both note the serum creatinine as well as the urine output in our patients in order to fully be able to diagnose kidney injury. 01:07 Now, what is our next step in looking at the patient? This is a really fun part of medicine because this is where we get to be a detective. 01:14 We're really looking at how to take a good history in our patients. 01:17 So for example, if I'm thinking my patient has an effective pre renal state or pre renal as a team Mia, I'm really looking for episodes where they might have prolonged hypotension. 01:26 This means when they have a decrease in perfusion to the kidneys and other vital organs. 01:31 I might see this in patients who are in shock, either basal dilatory shock from sepsis or cardiogenic shock, or perhaps in hemorrhagic shock after losing blood I might see this in my patients who have heart failure or Cardiorenal syndrome, and I may see this in patients who are volume depleted when they're just not getting enough intake to actually perfused their vital organs. 01:49 I mean, I also see the situation a bit because of medications or neurotoxic exposures. 01:55 This would include things like radio contrast exposure. 01:57 This is a type of media that we use in CT scans or angiograms, and it can be extremely toxic to the tubular portion of the kidneys. 02:05 Now, we don't always see this acute tubular necrosis for me, a contrast exposure is somebody who has underlying chronic kidney disease or an elderly patient who is coming in with volume depletion or in a diabetic with underlying CKD These patients are at very high risk when exposed to angiographic procedures once the injecting ratio contrast into the arterial circulation and that will be toxic to the kidney. 02:28 It causes basal constriction as well as tubular toxicity. 02:32 Acute tubular necrosis in our patients can happen. 02:35 We also discuss medications being toxic as well. 02:39 These include things like aminoglycosides, a very effective antibiotic, but at the same time it can cause acute tubular necrosis. 02:46 We see this with Amphotericin, a very effective antifungal agent, and we also see this with medications such as NSAIDs, which are infamous for impairing auto regulation. 02:56 So it can turn a situation that may have started out as an effective pre renal state into something that develops into tubular injury because of the prolonged ischemia changes. 03:05 We can also see things like a cycle of year that when given cause intra tubular crystal precipitation or I.V. 03:10 methotrexate, where that medication again and the volume depleted patient can actually crystallize within the tubules of the kidney We call that intra tubular obstruction. 03:20 Now, I'm also looking for medications that might be involved in the immune response that the kidneys can see, like an allergic interstitial nephritis These include medications like penicillins, cephalosporins and NSAIDs can cause this as well. 03:33 And I also see this sometimes with proton pump inhibitors these are medications that when taken, patients actually develop an immune response that can manifest with the type one or type four hypersensitivity reaction. 03:45 And when we end up with allergic interstitial nephritis, these patients oftentimes will manifest with white cells in their urine. 03:51 And we'll be talking about that a little bit later. 03:54 Now, the next thing we want to do is do a physical exam and remember how important physical exams are. 03:59 These are the signs that can really point us to the right diagnosis. 04:02 So our patient oftentimes holds all these answers. 04:06 The first thing I really like to do is to estimate the volume status of my patient. 04:10 I look at things like their neck in their face. 04:12 What does spectacular venous pressure look like? Do they have flat neck veins? Do they have poor skin trigger, or are they orthostatic when they stand up, or do they have hypertension? This would lead me to believe my patient is volume depleted Do they have very plump neck veins and elevated jugular venous pressure? Do they have peripheral edema? Am I thinking that my patient is perhaps in heart failure? That helped me to diagnose maybe a Cardiorenal syndrome? I also want to look for skin lesions that can help me. 04:41 These include things like rashes that we can often see in patients who have allergic interstitial nephritis. 04:46 Now, I'm not always lucky enough to see that because of the full triad of allergic interstitial nephritis, and the rash only happens in about 10% of cases. 04:54 But if I see a drug reaction, if I see a temporal correlation with the drug and X and some of the drug rash, perhaps peripheral eosinophilia and a fever, I'm thinking about allergic interstitial nephritis. 05:06 The other skin lesions that may help me is the patient who has undergone and aortic manipulation or they've had some kind of procedure where they have either injected dye or done some kind of procedure to the aorta or different arteries can actually dislodge a large amount of cholesterol crystals into their circulation. 05:22 So, for example, if my patient had an endovascular repair of a triple AA, then in that case those adenomatous crystals or cholesterol crystals cannibalized distally and end up in the arterials that cause renal disease just as they do with glomerular circulation. 05:36 They can do the same in skin circulation. 05:38 So we may see skin lesions that appear caused by microvascular ischemic changes from arterial occlusions caused by these cholesterol crystals that are embolization. 05:47 When I see that in the setting of maybe four to six weeks ago, my patient underwent in audit procedure. 05:53 This may guide my thinking. 05:55 Now, in addition to our physical exam, it's important for us to image our patients so we can really see what's going on in our patients who have the acute kidney injury. 06:03 If I'm worried about my patient having a post renal situation where they have obstruction of the urine, anywhere from the renal pelvis to the urethra, then imaging can be a very powerful tool for me to really clinch that diagnosis. 06:15 I can do something simple like an ultrasound when I can actually define the structural anatomy of the kidneys. 06:20 And if I see something like hyperhidrosis where I see dilatation of the pelvic system from urine that's backing up into the renal pelvis and actually the cortex, this tells me I may have obstruction. 06:29 It could be from somebody with an enlarged prostate like BPH or it could be from an obstructive stone or an obstructive lesion. 06:36 If I'm worried about a stone disease in my patient, I may want to get a non-contract CT scan to actually look for that intense density where I can actually see the obstruction of urine outflow from a stone or compression of the ureter from a tumor. 06:49 So imaging can be very powerful, particularly in situations where we're looking for post renal causes. 06:56 Now, the most important thing is really looking at the urine because oftentimes it holds many of the answers one's looking for. 07:02 One of the first things I like to look at for a patient when I'm considering, does this patient have an effective pre renal state or have they had an episode of prolonged volume depletion or they've developed ischemia? The test that may help me is called a FINA or fractional excretion of sodium. 07:16 It can be very helpful because of what it tells us is are the tubules intact and are the T-bills able to function? If we're an effective pre renal state, remember, our body is trying to hold on to all of the volume that it can in order to produce the vitals. 07:29 The renin angiotensin system is going to be activated when RAAS is activated, we are going to reabsorb every bit of sodium possible. 07:37 So we look at the fractional excretion of sodium. 07:39 It should be extremely low. 07:40 It's less than 1% in someone who is effectively pre renal and trying to hold on to volume. 07:45 But the tubules are still functioning. 07:47 This tells me the state my patient is in now. 07:50 Let's say my patient has a history of an effective pre renal state, but they have had volume depletion and a prolonged hypertensive state for such a long time that they've now developed injury to the tubules. 08:01 They may now have ATN in that situation. 08:03 The Tubules are no longer working effectively, and even though the RAAS is trying to be activated, it's not going to effectively work on the kidneys. And therefore I'll see sodium. 08:12 These tubules cannot reabsorb the sodium because they're injured in this situation. 08:17 My figure is going to be greater than 2%. 08:19 And remember that less than 1%, our patient is pretty renal. 08:23 They may be responsive to volume or we may have to look at Cardiorenal syndrome. 08:26 We have to correct their underlying cardiac function. 08:30 Now, in addition to looking at the FINA, I really want to look at the urine analysis. 08:34 The US or urine analysis are so important because they tell us whether there's protein blood of cells in the urine. 08:42 So just getting a routine urinalysis, either from a dipstick or from the lab, I can see whether my patient has proteinuria or hematuria. 08:49 If I see that I'm really thinking about glomerular disease and nephritis syndrome. 08:54 If my patient has leukocyte estimates or white blood cells or nitrates, that's really helpful and suggestive of a cute pyelonephritis or some kind of urinary tract infection. 09:03 So even just looking at the dipstick alone is very important and can give me some answers. 09:07 Now, one of my favorite things to do is actually look at the urine underneath the microscope because again, there's so many different things in there that can really help me clinch my diagnosis. 09:16 It's very satisfying, and I know how to treat my patient, like to do a microscopic exam, take ten. 09:21 Most of the patient's urine, centrifuged it at about 3000 RPMs for 5 minutes and then decant the supernatant. 09:27 I can take an actual pellet and resuspended that and look at that on the slide underneath the microscope at ten X or 40 X power. 09:34 When I do that, I see all sorts of things that are help me to diagnose my patient. 09:38 If I see crystals such as uric acid crystals, I might think my patient has a gout nephropathy or even something like tumor lysis syndrome, where they just have the rate that it's building up, causing obstruction in the tubules I may see calcium crystals in there that would suggest that my patient has a calcium oxalate stone, which is one of the most common stones seen in our patient population or it could be something like ethylene glycol toxicity that leads to calcium oxalate stones in the urine as well. 10:03 So again, you're very, very powerful in these situations with this information. 10:07 Now, probably what I see most commonly, it is going to be muddy brown casts or evidence of acute tubular necrosis. 10:14 And this is exactly what it looks like, these beautiful cylindrical shapes Of course, regular pigmented casts, also called Muddy Brown cast, really represent what's happening with acute tubular necrosis. 10:25 So think about this as the tubular epithelium is getting injured. 10:28 It undergoes apoptosis or necrosis. 10:30 When those cells are apoptosis, they get picked off from the underlying basement membrane and collect in the tubules where they combine to form this beautiful cylindrical cast that is pigmented with a granular appearance. 10:42 Those are then degenerated tubular epithelial cells. 10:44 And when I see this in a patient, I'm really thinking this patient has 18. 10:48 In my armament for diagnostic testing, I may even be lucky enough to see a free floating, tubular epithelia cell intact. 10:55 And when I see that, I'm really thinking about ATM. 10:58 Now, sometimes we also see white cell casts. 11:00 So again, if you look here at this picture, you can see the beautiful cylindrical shape here with the intact white blood cells embedded right into the cylinder or into the cast. 11:10 These are called white blood cell casts. 11:12 And again, what happens in patients who have inflammatory lesions such as allergic, interstitial nephritis or even in pyelonephritis, these white blood cells will collect in the tubule and they can bind with the urological protein and we get these cylindrical shaped casts. 11:26 So in white blood cell carcinoma, we can also see that in the urine, I think about this in the absence of bacteria. 11:32 But in the presence of bacteria, I think of some sort of infection or interstitial nephritis. 11:37 These are red blood cell casts and dysmorphic red blood cells in the left hand part of the slide. So if you look at the very left of the slide, we have beautiful red blood casts. 11:46 This is going to occur in the setting of nephrotic syndrome. 11:49 So again, red blood cells that collect within tubule lumen will combine with the urological proteins and form these beautiful cylindrical casts. 11:58 You can see that they have intact red blood cells and a little bit of brownish red hue. 12:02 And that tipped me off that this is in fact a red blood cell. 12:05 Sometimes I'm not lucky enough to see these red blood cell casts, but what I will see are these dysmorphic red blood cells, and that's pictured in the middle of the slide. 12:13 And what happens is in these nephrotic syndrome patients, these red blood cells traverse the glomerular basement membrane. 12:19 And as they do this, they become to form and develop blood on their membrane. 12:23 This is what you can see here. 12:25 Now, interestingly, the top right corner, you see what looks like a Mickey Mouse. 12:29 We sometimes refer to these affectionately as Mickey Mouse cells that we see in our patients who have dysmorphic red blood cells. 12:34 And again, this is suggestive of glomerular disease. 12:38 Now, finally, in some of our glomerulonephritis patients, we actually see white blood cell Cas. 12:43 I spoke about this when I was talking about acute interstitial nephritis or in the presence of a positive bacterial culture pyelonephritis. 12:49 So finally, if we're looking at sediment and we see isolated white blood cells or pyrite, we usually think about infection. 12:56 But this can also occur in noninfectious cases, such as a sterile culture, a nitrate, negative dipstick. 13:02 And at this time, you want to think about things like interstitial nephritis. 13:05 Now, if on the other hand, I see a normal urinalysis with few cells or no cars, this is normally considered boring for a nephrologist, but probably better for the patient. 13:14 And with this, there may be only a few cells here there, but no real cellular casts or any true highlighted casts. 13:20 In these cases, we think about pre renal disease, urinary tract obstruction, in hypercalcemia acute phosphate nephropathy or myeloma cast nephropathy. 13:29 In certain cases, it may be necessary to do a renal biopsy in these patients to confirm your diagnosis. 13:34 And with that, you've made it to the end of the lecture. 13:36 Congratulations.
About the Lecture
The lecture Algorithm of Acute Renal Injury by Carlo Raj, MD is from the course Tubulointerstitial Diseases.
Included Quiz Questions
What is the next step in management for a patient presenting with azotemia?
- Renal ultrasound
- Microalbuminuria dipstick
- Urine specific gravity
- Urine culture
- Glucose dipstick
What pathology is most likely responsible for azotemia in a patient presenting with hydronephrosis?
- Post-renal obstruction
- Pre-renal ischemia
- Chronic renal failure
- Glomerulonephritis
- Renal artery stenosis
Which of the following is the most likely pathology in a patient with normal-sized kidneys on ultrasound with WBC casts and eosinophilia on urinalysis?
- Interstitial nephritis
- Acute tubular necrosis
- Minimal change disease
- Pre-renal ischemia
- Post-streptococcal glomerulonephritis
Which of the following test results would be expected in a patient with chronic renal failure?
- Isosthenuria
- Protein > 3.5 g/d
- Urine osmolality > 500 mOsm/L
- Renomegaly
- RBC casts
Which of the following is the most likely pathology in a patient with small kidneys on ultrasound and protein < 3.5 g on urinalysis?
- Chronic renal failure
- Acute tubular necrosis
- Acute interstitial nephritis
- Pyelonephritis
- Nephrotic syndrome
Which of the following is most likely in a patient with normal-sized kidneys on ultrasound and with RBC casts and proteinuria on urinalysis?
- Glomerulonephritis
- Pyelonephritis
- Interstitial nephritis
- Pre-renal azotemia
- Chronic renal failure
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Lecturio is a solid and highly efficient learning Platform. Dr. Raj is a seasoned communicator, and has just the right balance of serious professional demeanor, clarity of speech and concepts, and good humor you want in a Teacher. This lecture, like the others I’ve watched so far, is excellent stuff!