Playlist
Show Playlist
Hide Playlist
Alagille Syndrome
-
Slides Conjugated Hyperbilirubinemia and Liver Diseases Pediatrics.pdf
-
Download Lecture Overview
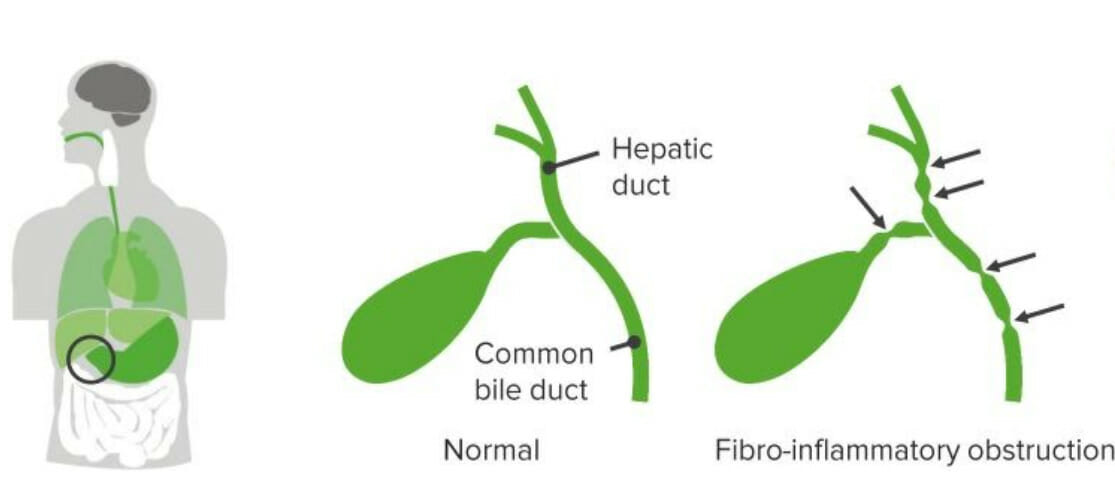
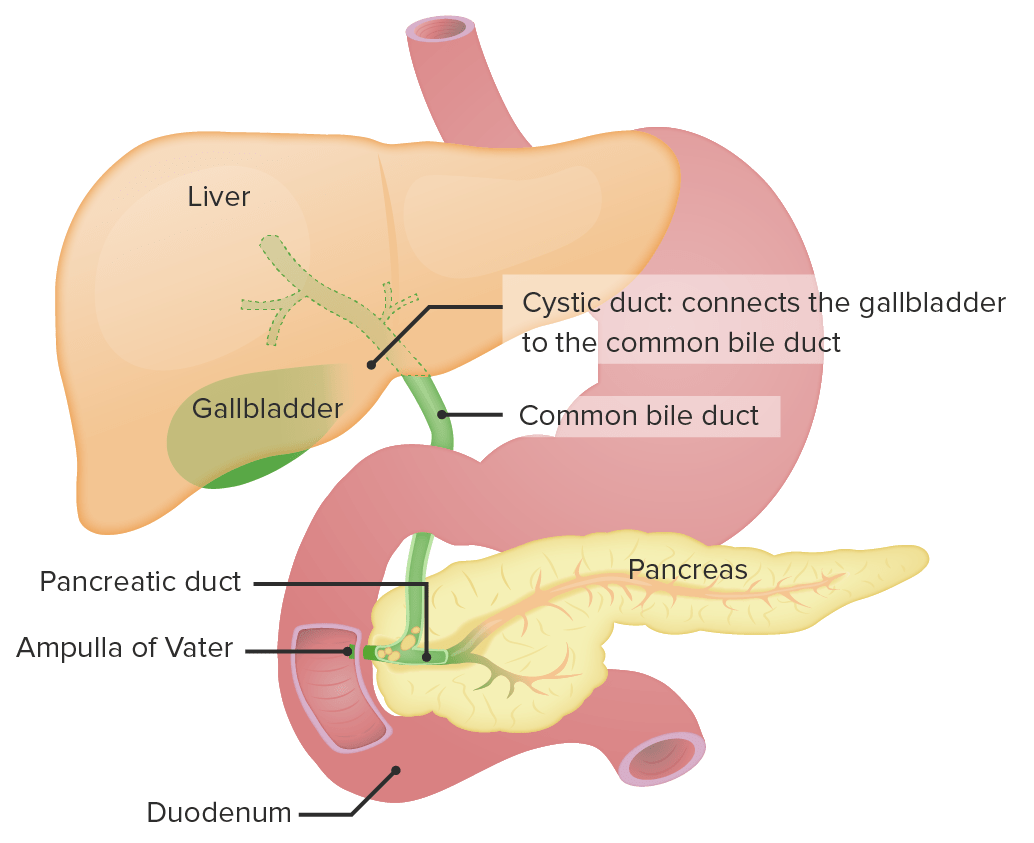
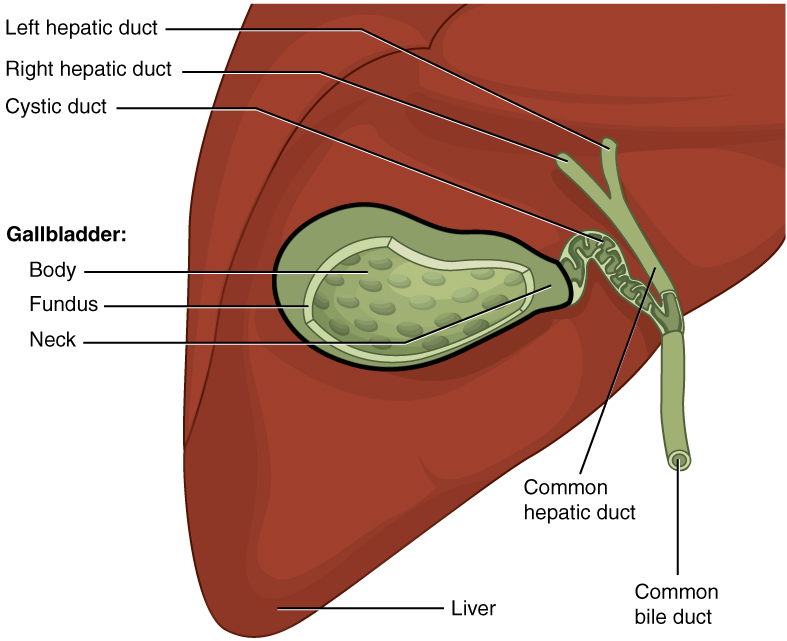
00:01 Okay, so let’s start to look at some of these problems one at a time and try and identify what could be the cause of a child’s conjugated hyperbilirubinemia. 00:14 Here’s an example. A neonate is born and has persistent direct hyperbilirubinemia and you notice syndromic abnormal facies. 00:25 What should you suspect? The answer is Alagille Syndrome. 00:30 Let’s look at Alagilles a little bit more carefully. 00:33 The signs and symptoms of Alagilles are generally related to a number of different organs that can be involved. 00:42 First, we will see cholestasis in these children. 00:45 They will have a conjugated hyperbilirubinemia and that cholestatis may result in liver problems as well. 00:53 Frequently these children’s have congenital heart disease, something like Tetralogy of Fallot, so a murmur is often appreciated. 01:02 And lastly these children can develop posterior embryotoxon in the eye which may cause problems down the road and it’s something that you have to watch out for. 01:13 So here are some examples of some patients with syndromic facies consistent with Alagille’s. 01:20 You can notice triangular facies, a large prominent forehead, a wide nasal bridge, a small pointed chin and deep set eyes. 01:29 These are all findings consistent with the Alagille Syndrome. 01:33 This diseases is autosomal dominant. It’s a defect in the short arm of chromosome 20 on 20p12 and they usually have de novo mutations, that is to say, the parent doesn’t have alagille’s this is a new mutation, but absolutely you wanna get a family history as well. 01:55 What you’ll find on these patients if you were to biopsy them is a paucity of interlobar bile ducts including hepatic development leading to cholestasis and you can see that around the bile ducts we have some inflammation here and some problems. 02:11 So let’s look at how we would make a definitive diagnosis. 02:17 Typically in these children we need to see three out of five physical features. 02:22 We need to see evidence of cholestasis and then we’ll usually end up doing a liver biopsy on these children. 02:30 For patients with mild disease, we’ll treat them with ursodeoxycholic acid. 02:35 This helps facilitate bile flow through the abnormal biliary tract and allows the liver to not be so backed up. 02:44 Remember, the patients with liver failure may develop pruritus or itching and it can be very severe and generally we’ll treat that symptomatically with an antihistamine like diphenhydramine or Benadryl. 02:57 For patients with severe disease they often proceed to liver transplant. 03:02 Remember, that in patients with this problem, they are going to have a decrease of ability to absorb fat soluble vitamins. 03:13 These children require extra supplementation of the fat soluble vitamins A, D, E, and K and they also often get zinc as well.
About the Lecture
The lecture Alagille Syndrome by Brian Alverson, MD is from the course Pediatric Gastroenterology.
Included Quiz Questions
Which of the following liver biopsy findings is generally seen in patients with alagille syndrome?
- Paucity of interlobular bile ducts
- Ductal proliferation
- Onion skinnng
- Sinusoidal mononuclear cell infiltration
- Kupffer cell hyperplasia
Which of the following is not a feature of Alagille syndrome?
- Cleft lip
- Congenital heart disease
- Cholestasis
- Posterior embryotoxon
- Pointed chin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Important topic in pediatrics. Very clear explanations. Thank you very much!