Playlist
Show Playlist
Hide Playlist
Acute Stroke: Evaluation and Workup
-
Slides 01 Stroke Neuropathology I.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
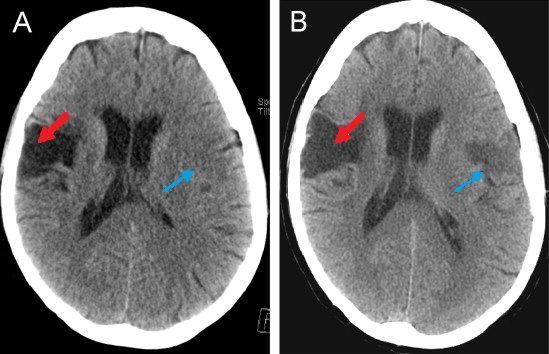
00:01 Now, acute stroke evaluation and workup. 00:04 How are you going to work up your patient as you go through and you suspect stroke? ABCs, we’ll talk about these. 00:12 And in the NIH, they have laid out a stroke scale and there’s a particular chart and table that I’m giving you with that scale, just have a general overlook and you’ll see what I’m referring to when I get to it. 00:26 Do not spend time memorizing every single line of that particular scale. 00:31 Don’t worry, I’ll walk you through that. 00:33 Others. 00:34 Other workups that you want to keep in mind, glucose, CBC, PT/PTT. 00:39 On the head CT, what are you looking for? Well, maybe look for hemorrhage. 00:43 And we're here, once again, you try not to use contrast, if you already know that there's a possibility of increased intracranial pressure, then you don't want to use contrast, please. 00:52 MRI, I'll talk about this in a second. 00:55 Clues about the ischema. 00:57 A good example would be the middle cerebral artery dot sign, Edema, could you find edema with your head CT? And here with the middle cerebral artery, I'm going to quickly walk you through what becomes important for you is a little bit of a timeline. 01:13 And just to be clear, with the head CT, if you find minimal involvement of the brain, let's say that your patient has having aphasia, okay. 01:22 And you're suspecting that the middle cerebral artery is the issue and your patient has a history of hyperlipidemia diabetes, so on and so forth. 01:32 The MCA consists of different segments. 01:35 More inferior, the M2 segment of the MCA can be viewed longitudinally in a single axial slice on a CT scan. 01:44 If the thromboembolus takes place in that segment, then hyperdense MCA will be seen. 01:51 If the occlusion occurs on a more superior segment of the MCA, the part that goes to the insula, then you will see the dot sign. 01:59 This happens because now you are seeing a cross sectional section of the MCA segment that is perpendicular to the axial orientation of the CT slices. 02:10 Both signs are seen in the first 90 minutes post stroke. 02:15 Both of them appear as hyperdense and white. 02:19 Rush, ischemic stroke treatment. 02:24 Now, here, this is important, time to tPA administration, less than 4.5 hours from the onset of the symptoms. 02:34 So this is where your imaging studies are going to become incredibly crucial. 02:39 Granted, in current day practice, there are many, many advancements in imaging and such. 02:45 But at this point, something that I walked you through is the noncontrast CT. 02:50 And where for example, I gave you middle cerebral artery type of stroke, and what it means for one hour. 02:57 So really pay attention to 4.5 hours, please, with TPA. 03:03 An MRI and MRA, which is Magnetic Resonance Imaging, or angiography. 03:08 This would be DW-Imaging or diffuse weighted. 03:11 And this gives you a little bit more detail about the tissue. 03:14 But at this point, it is important that you pay attention to the CT with the quick little timeline that I'm going to provide for you. 03:22 So as I was saying earlier, with the NIH stroke scale, I want to give you this table so that you have it readily available. 03:30 And just go through the first column here on your own time, and ever so often just come back and refer to this, it's not important that you memorize every single line that is never going to be asked. 03:41 But in general, you know, when is the loss of consciousness taking place? What are the risk factors, and so on and so forth? And this then gives you a scale for that type of stroke that the NIH has provided. 03:56 Now, what you'll notice here on the CT is an area of hyperdense. 04:00 And you'll notice that it is the parietal lobe or lateral hemisphere that is affected. 04:05 And so therefore, it should clue you in that the middle cerebral artery is in fact the culprit. 04:10 And if it is atherosclerosis, that setting in here, shall we say, then a patient presents with aphasia, or motor type of issues. 04:19 And it's the, remember the upper extremities so you're thinking about the face, and arms, and such, then you know that it probably more of the dominant side. 04:28 Non-dominant side, you should be thinking more like more or less of what's known as your hemineglect. 04:33 Quickly here, all that I wish to show you upon, noncontrast CT. 04:39 These are noncontrast CT images that I'm giving you only. 04:42 The MCA dot sign, seen here in the Sylvian fissure, is the cross-sectional equivalent of the hyperdense MCA sign. 04:50 In 24 hours, you will notice please on the lateral hemisphere of the brain, that there is a large area in which it has undergone your atherosclerotic type of ischemic stroke. 05:02 And so, therefore, the brain is being affected, is hypodense, and this is approximate 24 hours later. 05:09 Now, what you also want to keep in mind as you go through the timeline is, well, how did this occur? Was it atherosclerosis? Also keep in mind that with MCA, if you're adjoining or if you're coming to your entry supraartery, and you have a tissue in which both the blood vessels are supplying that part of the brain, this is then referring to your watershed area. 05:32 Things that you want to keep in mind. 05:35 Post-Acute Stroke Workup. 05:36 MRI/MRA, cholesterol levels, TSH, syphilis, such as RPR. 05:43 Always keep in mind B12, homocysteine or erythrocyte sedimentation rate. 05:48 Echocardiogram as to whether or not the issue was in the heart, carotid ultrasound. 05:53 Specialized tests, remember, that you could have some of the issues that are taking place risk factors such as hypertension, diabetes. 06:01 We talked about those that more or less would be the risk factors such as tobacco versus genetic. 06:09 And if it was genetic, such as your CADASIL, an autosomal dominant type of stroke like issue leukoencephalopathy, then do a skin biopsy. 06:18 And this will then help you with diagnosing CADASIL, or hypercoagulable workup. 06:24 What do we mean by this? Remember, we talked about antiphospholipid syndrome, and so therefore, you're looking for that lupus anticoagulant. 06:32 You have female, multiple miscarriages. 06:34 Or we talked about potency deficiency or Factor V Leiden, a very, very, it is the most common hereditary genetic type of hypercoagulable state. 06:43 Keep all that in mind as you go through workup so that you know exactly as to how your stroke is developed.
About the Lecture
The lecture Acute Stroke: Evaluation and Workup by Carlo Raj, MD is from the course Stroke (Cerebrovascular Accident). It contains the following chapters:
- Acute Stroke Evaluation and Workup
- NIH Stroke Scale
- Post-Acute Stroke Workup
Included Quiz Questions
What is an essential test in the initial workup of a patient with a stroke?
- Head CT
- D-dimer
- Urinalysis
- Antiphospholipid antibody
- ESR
Which test is contraindicated in a patient presenting with stroke and signs of intracranial hemorrhage?
- Head CT with contrast
- Head CT without contrast
- Head MRI
- Head MRA
- PT/PTT
What is the most likely finding in a non-contrast head CT of a patient presenting two hours after the onset of stroke involving the M2 segment of the middle cerebral artery (MCA)?
- Hyperdense MCA sign
- Hypodense MCA sign
- Pseudo-delta sign
- Diffuse hemorrhage
- Thalamic infarct
After the onset of a stroke, what is the approximate duration for the "MCA dot sign" to appear on a non-contrast head CT?
- 90 minutes
- 24 hours
- 60 minutes
- 30 minutes
- 45 minutes
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |