Playlist
Show Playlist
Hide Playlist
Acute Shoulder Pain: Management
-
Slides AcuteShoulderInjury AcuteCare.pdf
-
Download Lecture Overview
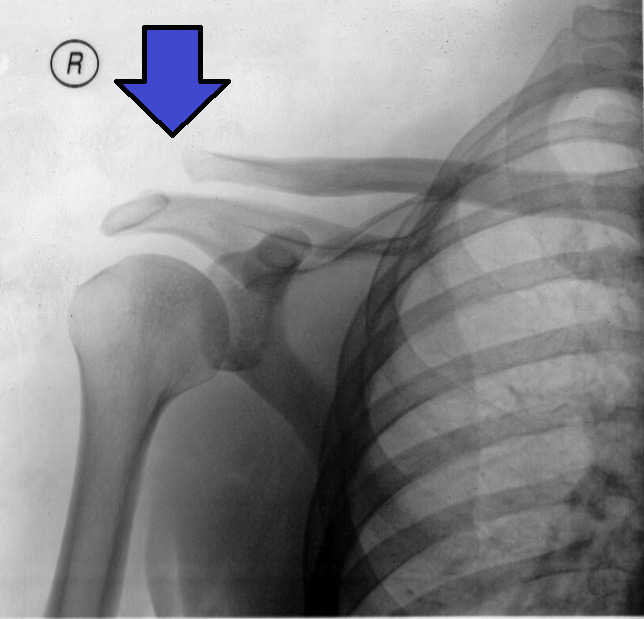
00:01 I don't routinely do plain radiographs or other imaging studies on that first patient visit. 00:09 A lot times, those provocative tests will lead me towards a probable diagnosis. 00:13 And many of these disorders do work out over time, so therefore I'm just going to provide supportive care until it does. 00:20 When the pain becomes more chronic, if this patient gets – for example, who's had pain for four weeks, does not get better on our initial recommendations alone, certainly I’ll recommend x-rays for her next time. 00:32 And in general, when we talk about musculoskeletal medicine, I think MRI is a great tool, but I use it really when we’re thinking about intervening in a case with some kind of active intervention. 00:43 So, that’s referring on to a procedure such as injection therapy in or around the joint and/or surgery. 00:53 So, what about just the general management of shoulder pain? So, modification activity is really important. 01:00 Should not keep your – your shoulder should not be raised above your – like above 90° in abduction or flexion when working. 01:09 And if patients do a lot of overhead activity, they work cleaning houses, they work in a stock room, they need a ladder because working over your head all day will give you shoulder pain every time eventually. 01:24 Simple analgesics, whether this patient chose ibuprofen and acetaminophen, they are more similar than they are different. 01:31 Again, I always am concerned with the safety of NSAIDs used over time. 01:36 Over a couple of weeks, particularly in a young healthy patient, is not going to make a difference. 01:39 Used over two years, there's a big separation between acetaminophen being more safe than NSAIDs. 01:46 Injections, commonly used. 01:48 I do them. 01:49 I approve them. 01:50 We use corticosteroids. 01:52 There is very little data to support the practice, but they've been used for many, many years. 01:58 It's important to give a probable diagnosis because there are some different sites you can inject, the most common being a subacromial bursa injection which will take care of particularly adhesive capsulitis fairly well, but also can improve rotator cuff tendinitis. 02:13 But if you really are suspecting biceps tendinitis, different area for injection, here in the interior and the bicipital groove. 02:21 Or if – particularly if you demonstrate acromioclavicular joint arthritis, different form of injection, again into the AC joint. 02:29 So, think about that as you’re forming your differential because it's going to dictate where you might put in injections. 02:34 And overall, the best evidence for injections in terms of what I think they can improve most effectively is adhesive capsulitis. 02:40 That loss of range of motion that this patient probably – if we think back to our case, she had had four weeks of pain in her shoulder, started with just pain. 02:50 Now, she's having stiffness and she’s probably developing adhesive capsulitis on top of what I would guess would be a rotator cuff tendinitis. 02:59 If these things don't work, there’s physical therapy. 03:01 There’s also surgical referral. 03:03 And I'll probably think about an MRI if it's that severe that she needs to go to surgery. 03:10 So, hopefully, you’ve gained an appreciation for the common differential diagnosis of the pain in the shoulder joint. 03:19 We went through some of the physical exam, particularly the provocative testing. 03:23 And then the therapy isn't that dissimilar from other forms of musculoskeletal medicine, with an important focus on limitation of exacerbating activities, particularly working overhead, and thinking of using injections based on what you found on physical examination. 03:40 Thank you.
About the Lecture
The lecture Acute Shoulder Pain: Management by Charles Vega, MD is from the course Acute Care.
Included Quiz Questions
A 42-year-old man presents to your office with persistent shoulder pain. He was diagnosed with rotator cuff tendinitis 3 months ago. His medications include ibuprofen. He has had appropriate modification of activity and physical therapy. Which of the following is the most appropriate next step in diagnosis/management?
- Imaging
- Joint injection
- Tramadol
- Referral to a surgeon
- Continued physical therapy and analgesics
Which of the following is the most appropriate initial therapy for biceps tendinopathy?
- Modification of activity
- Joint injection
- Opiates
- Surgical referral
- Shoulder X-ray
Intraarticular injection of glucocorticoid and anesthetic is most appropriate in the treatment of moderate to severe symptoms of which of the following conditions?
- Adhesive capsulitis
- Proximal long biceps tendon tear
- Acromioclavicular joint degeneration
- Chronic supraspinatous tendinopathy
- Chronic infraspinatous tendinopathy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |