Playlist
Show Playlist
Hide Playlist
Acute Pancreatitis with Case
-
Slides Gastroenterology 18 Pancreas Disorders.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
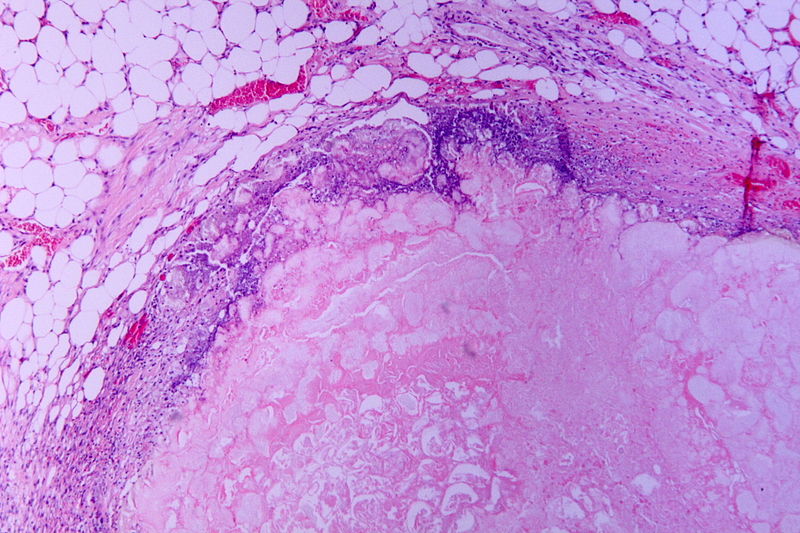
00:00 Welcome. Today we will discuss disorders of the pancreas. 00:05 So, we'll begin right away with a case. 00:08 A 38-year-old man is evaluated in the ED for acute epigastric pain. 00:14 The pain began four hours ago, radiates to the back and is associated with nausea and bilious vomiting. 00:20 He has no medical conditions. He drinks six beers a day. 00:24 Vitals are notable for a heart rate of 110 and a respiratory rate of 25. 00:29 He has epigastric tenderness without guarding or rebound. 00:33 Bowel sounds are hypoactive. No jaundice is noted. 00:37 His lab studies reveal a white cell count of 18,000 and a serum lipase of 1600. 00:44 Abdominal ultrasound shows a normal gallbladder without biliary dilatation. 00:49 What are the best initial steps in management? So let's look at some key items in this case. 00:55 He has acute abdominal pain radiating to the back. 00:59 And he's a patient with known alcohol use disorder. 01:02 In addition, his vitals are notable for tachycardia and tachypnea. 01:07 And he has leukocytosis indicating SIRS or systemic inflammatory response syndrome. 01:13 His labs otherwise are notable for an elevated serum lipase. 01:18 And he has a normal gallbladder on his ultrasound. 01:22 So, before we talk about management, let's talk about acute pancreatitis. 01:28 How does acute pancreatitis occur? So, the pathogenesis of pancreatitis begins with an obstruction of the pancreatic duct or some trigger for pancreatic inflammation. 01:41 Blockage of the pancreatic duct to then leads to premature activation of the pancreatic enzymes that are normally secreted to help with digestion. 01:50 When these enzymes are secreted and they have nowhere to go, they then begin to auto digests the pancreas and create a lot of local inflammation. 02:01 This then can contribute to capillary leak syndrome and ultimately SIRS or systemic inflammatory response syndrome which can appear as like sepsis. 02:12 And in the worst-case scenario can develop multi-organ failure. 02:17 There are many different causes of acute pancreatitis. 02:22 One mnemonic that I find helpful and that you will probably will encounter is the, IGETSMASHED mnemonic. 02:29 This stands for idiopathic, gallstones, ethanol and trauma and all of the etiologies you see here. 02:36 Note that about 80% of all cases are related to gallstones and ethanol. 02:44 If you don't remember this mnemonic, note that there are many causes that are listed here for your reference. 02:50 I will point out that many medications can cause pancreatitis some of which include hydrochlorothiazide, furosemide and azathioprine, so all medications that can be used commonly. 03:02 And infections can also cause pancreatitis including mumps, Coxsackie virus and cytomegalovirus. 03:09 So, the symptoms of acute pancreatitis usually include, severe upper abdominal pain which often radiates to the back because of the anatomic location of the pancreas. 03:20 Patients may present with fever and nausea and vomiting as well. 03:25 The diagnosis is made based on having at least two of the three following clinical criteria. 03:33 So, they must have an acute onset of upper abdominal pain. 03:38 They may also have a serum amylase or lipase greater than three times the upper limit of normal. 03:45 Or they may have characteristic findings of pancreatitis on imaging which can be either a CT with contrast, an MRI or ultrasound. 03:56 Here on the right, you can see an example of a CT of the abdomen showing acute pancreatitis. 04:02 So you see an edematous or swollen pancreas with adjacent fat stranding around it. 04:08 This is typical of acute pancreatitis on CT scan. 04:12 As a quick high-value care aside, you should not check for both amylase and lipase when you suspect acute pancreatitis. 04:23 A serum lipase is enough to make the diagnosis because it has better sensitivity and is elevated for longer than the amylase. 04:31 So just remember when faced with acute pancreatitis, just test for lipase. 04:37 So, now let's talk about the treatment and scoring severity of for acute pancreatitis. 04:43 There are several severity scoring systems we can use to help us determine a patient's prognosis. 04:49 They include the Apache II system and Ranson's criteria. 04:54 I'm not gonna go into detail about what they include, but you can easily look them up. 04:59 So, with this, we should provide aggressive fluids. 05:03 The management of acute pancreatitis has changed over the years. 05:07 You should remember that in pancreatitis, because of all of the inflammation occurring in the pancreatic tissues is similar to having a severe burn inside the body. 05:17 The mainstay of treatment used to be aggressive IV fluid resuscitation, around 250-500 cc/hour of crystalloid fluids. 05:27 However, since the WATERFALL trial in 2022, we found that moderate fluid resuscitation may be better at preventing fluid overload. 05:36 The guidelines continue to evolve, but the recommendation is to give a bolus of 10 cc/kg of body weight in patients with hypovolemia, followed by an infusion of 1.5 cc/kg per hour of lactated Ringer's solution. 05:52 The choice of crystalloid fluid is also important. 05:55 Lactated Ringer's solution can reduce the incidence of systemic inflammatory response or SIRS, when compared to normal saline. 06:04 So, with this, we should provide aggressive fluids. 06:08 You also want to offer the patient to have a brief period of bowel rest. 06:14 Keep in mind that once the patient feels a little bit better and their nausea, vomiting and abdominal pain have improved, you can safely restart oral feeding. 06:23 If they continue to feel terribly and they're not able to eat after 72 hours, then evidence shows that starting enteral nutrition by either a nasogastric tube or a nasojejunal tube can improve the patient's outcome. 06:39 A third element of management is offering pain control as patients often have very severe pain. 06:46 And lastly, you want to also give antiemetics to help them with their nausea. 06:51 So, there are many complications that can occur from acute pancreatitis. 06:56 The first one is just a peripancreatic fluid collection. 07:00 This can happen early in the course of pancreatitis and usually resolved spontaneously. 07:06 So no special management is needed. 07:09 On the other hand, you may develop a pancreatic pseudocyst which occurs usually about four weeks or more after the first episode of pancreatitis and it is a persistent collection of fluid around the area. 07:22 We usually manage this by just observing the pseudocyst but if the patient becomes symptomatic or there is rapid enlargement of the pseudocyst, you may drain the pseudocyst. 07:35 The next complication is necrotizing pancreatitis. 07:40 This is when there is such severe inflammation that patients develop necrosis of the pancreas and any adjacent tissues. 07:47 This makes them also at very high risk for developing an infection to the area. 07:52 So, we manage them with providing broad-spectrum antibiotics if they deteriorate clinically. 07:59 Because of all of the local inflammation, patients may also present with splanchnic venous thrombosis. 08:06 So you may have a clot form and any of the veins surrounding the pancreas including the splenic vein, portal vein or the SMV. 08:14 The management is purely by treating the underlying inflammation or pancreatitis. 08:19 And lastly, one of the most dreaded complications of acute pancreatitis is abdominal compartment syndrome. 08:27 This is when the amount of inflammation within the abdomen has exceeded the pressure. 08:32 So, an intra-abdominal pressure of greater than 20 mmHg along with organ failure. 08:40 And we manage these patients with supportive care. 08:43 In very severe cases, we may need to do surgical decompression which involves opening the abdomen to allow relief of the high-pressure. 08:52 So, we can now talk about all of these complications in terms of imaging. 08:56 On imaging, you may see necrotizing pancreatitis shown here with an area of walled off necrosis. 09:04 The second thing you may see is a large collection of dark color fluid as shown here. 09:10 This -- if you see this after about four weeks after the initial pancreatitis episode, would be a pancreatic pseudocyst. 09:18 Next, you may see a specific type of splenic vein thrombosis leading to infarct of the spleen. 09:26 Here, you can see on the very innermost tip of the spleen a small area of darkening which is the area that has been infarcted because of a thrombosis. 09:38 And lastly, you may see evidence of ascites on imaging. 09:42 So here on CT, the dark areas of fluid in the free abdomen or peritoneum represents ascites. 09:50 So now let's return to our case. 09:55 We had a 38-year-old man who has now acute abdominal pain radiating to the back. 10:00 He has known alcohol use disorder. 10:02 He has SIRS or the systemic inflammatory response syndrome and an elevated serum lipase with a normal gallbladder on ultrasound. 10:11 So, if we put this all together, we can suspect that he has acute pancreatitis from his underlying alcohol use. He now has SIRS. 10:19 And importantly, since his gallbladder looks normal on ultrasound without any gallstones, we know that the alcohol was likely the trigger for his pancreatitis. 10:29 So the best initial steps in management include giving IV fluids (and lactated Ringer's is preferred), and allowing for a brief period of bowel rest, so keeping patients NPO until they are able to tolerate food without vomiting or ileus. Also you can offering pain control, and antiemetics
About the Lecture
The lecture Acute Pancreatitis with Case by Kelley Chuang, MD is from the course Disorders of the Pancreas.
Included Quiz Questions
Which of the following risk factors accounts for the majority of cases of acute pancreatitis?
- Gallstones
- Trauma
- ERCP
- Hypertriglyceridemia
- Autoimmune inflammation
Which of the following is part of the diagnostic criteria for acute pancreatitis?
- Serum amylase or lipase >3 times the upper limit of normal
- Chronic abdominal pain
- Serum lipase or amylase >2 times the upper limit of normal
- Fever
- Tachycardia
Which of the following is the treatment of choice for acute pancreatitis?
- Moderate fluid resuscitation and bowel rest
- Surgery
- Antibiotics
- Laxatives
- Proton pump inhibitors
Which of the following is the treatment of choice for necrotizing pancreatitis?
- Broad-spectrum antibiotics
- NSAIDs
- Observation
- Ligation
- Antacids
Which of the following medications is a risk factor for pancreatitis?
- Hydrochlorothiazide (HCTZ)
- NSAIDs
- Proton pump inhibitors
- Octreotide
- Sotalol
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Chuang explains management and treatment well and provides more detailed information in the Q&A which is helpful for understanding and solidifying the lesson.
1 customer review without text
1 user review without text