Playlist
Show Playlist
Hide Playlist
Acute Mesenteric Ischemia with Case
-
Slides Gastroenterology 09 Disorders Large Intestine II.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
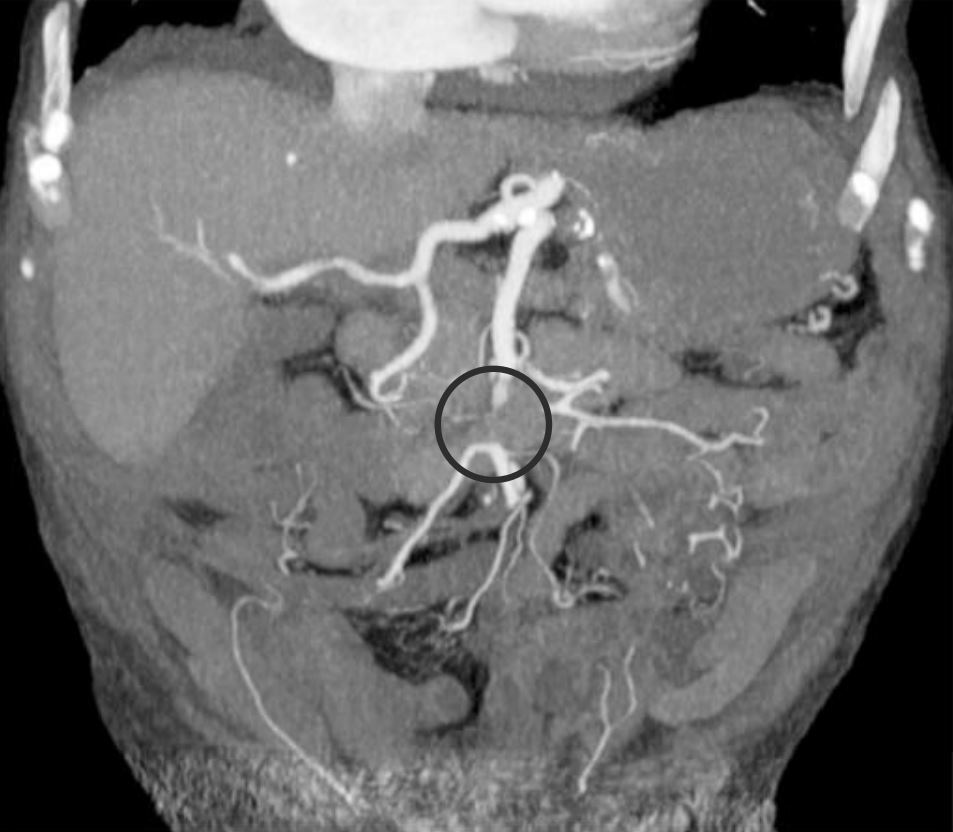
00:01 Welcome. 00:01 Today we'll talk about further disorders of the large bowel. 00:06 So we'll begin with a case We have a 78-year-old man who was hospitalized for pneumonia. 00:12 He has a history of coronary artery disease and peripheral artery disease with chronic ulcers on his left lateral ankle. 00:20 On hospital day 2, he suddenly develops severe abdominal pain and watery diarrhea. 00:25 Vitals are notable for an irregularly irregular pulse of 130 and a blood pressure of 92/55 On abdominal exam, he has mild tenderness in the lower quadrants without rebound tenderness. 00:39 His rectal exam shows light brown stool. 00:42 Labs show a leukocyte count of 11,000 and lactate of 6 EKG shows atrial fibrillation and a stool PCR for C. difficile is negative. 00:54 What is the most likely diagnosis? So let's go through some key clinical features. 01:00 He has a history of known atherosclerotic disease and he's now presenting with sudden onset severe abdominal pain with diarrhea. 01:09 He does have a history of atrial fibrillation as by his physical exam and confirmed on EKG. 01:16 And interestingly, although he describes severe abdominal pain, on exam, he just has mild tenderness. 01:22 This is described as abdominal pain out of proportion to his exam findings. 01:29 And he has a high white count and an elevated lactate which are both somewhat concerning. 01:37 Lastly, he has a negative C.difficile PCR. 01:40 This is helpful because in a patient coming in with abdominal pain and diarrhea who's been hospitalized, you would worry about C. difficile infection. 01:48 But a negative test is reassuring. 01:52 So before we answer that question, let's look at some key clinical clues and put them all together. 01:58 Let's think, what condition is associated with sudden onset abdominal pain out of proportion to physical exam and a history of atrial fibrillation with atherosclerotic disease. 02:11 So you might be thinking of mesenteric ischemia This is when you have a decline which can be either acute or chronic in your arterial or venous intestinal blood flow. 02:23 So, we'll have to recall our anatomy of blood flow to the colon Recall that the aorta is the largest vessel in your body that supplies blood elsewhere. 02:33 You have your superior mesenteric artery or the SMA that supplies a large portion of the colon and the inferior mesenteric artery or the IMA which supplies the rest of the colon. 02:45 So mesenteric ischemia can either be acute or chronic. 02:49 When it is acute, it is a vascular emergency with a very high mortality rate It usually results from an acute embolism or an arterial thrombosis but there are other causes we'll go into next. 03:02 It can also be chronic which is a more long standing process commonly due to underlying athersclerotic disease. 03:11 So let's talk in detail about acute mesenteric ischemia. 03:15 It results from an acute drop in the perfusion to the intestine and as we mentioned before has a very high mortality rate of around 60% It can be from an embolism, a thrombosis or a non-occlusive ischemia and patients will present with sudden abdominal pain out of proportion to physical exam They may have anorexia or loss of appetite, vomiting or peritonitis in various severe cases. 03:45 The diagnosis is made by angiography. 03:47 This can be either through CT angiography or interventional angiography. 03:52 Here on the right, you see an example of CT angiography In this case, you can see a cut-off of the blood flow in the mid portion of the superior mesenteric artery. 04:03 This is likely from an occlusive embolism in this case. 04:07 So treatment, is with primarily supportive therapy, so giving IV fluids, avoiding medications that will cause further vasoconstriction to the area, and providing broad spectrum antibiotics. 04:21 You may also then do an embolectomy or surgery if necrotic bowel has formed. 04:29 So as we mentioned, there are several types of acute mesenteric ischemia. 04:34 The first is an arterial embolus, most commonly it's from cardiac origin due to any of these cardiac condition listed here. 04:43 You may also get an acute thrombosis on top of overlying atherosclerotic disease. 04:52 A third mechanism is non-occlusive mesenteric ischemia. 04:56 This is when in general, you just have vasoconstriction of your splanchnic vessels, due to low cardiac output or medications that are causing vasoconstriction. 05:06 And lastly, you may also have a venous thrombosis. 05:10 Most commonly this occurs in hypercoagulable states, so in settings like infection, severe inflammation as with pancreatitis, medications that cause this, or cancer. 05:24 So now that we've gone through that, let's return to our case. 05:26 We have our 78-year-old man with known atherosclerotic disease who now has sudden onset severe abdominal pain. 05:34 He has a known history of atrial fibrillation. 05:36 And on exam, he has abdominal pain out of proportion to the findings. 05:41 Importantly, we have already ruled out C. difficile infections since that is a thing on your differential. 05:48 So, you should now recognize this clinical constellation of symptoms in the setting of his known atherosclerosis and A.fib which would prompt you to a diagnosis of an acute mesenteric ischemia likely from a cardiac embolus.
About the Lecture
The lecture Acute Mesenteric Ischemia with Case by Kelley Chuang, MD is from the course Disorders of the Small and Large Intestines.
Included Quiz Questions
Which of the following is the best diagnostic test for acute mesenteric ischemia?
- CT angiography
- Abdominal X-ray
- Abdominal ultrasonography
- Endoscopy
- Colonoscopy
Which of the following is the best next step after IV fluids and antibiotic initiation in a patient with acute mesenteric ischemia?
- Surgery to resect necrotic bowel
- Vasoconstrictors
- Fluid restriction
- Diuretics
- Diet
Which of the following can cause arterial embolism and result in acute mesenteric ischemia?
- Atrial fibrillation
- Pancreatitis
- Malignancy
- Vasoconstrictor medications
- Atherosclerotic disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |