Playlist
Show Playlist
Hide Playlist
Acute Hypoxemic
-
Slides RespiratoryFailure RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
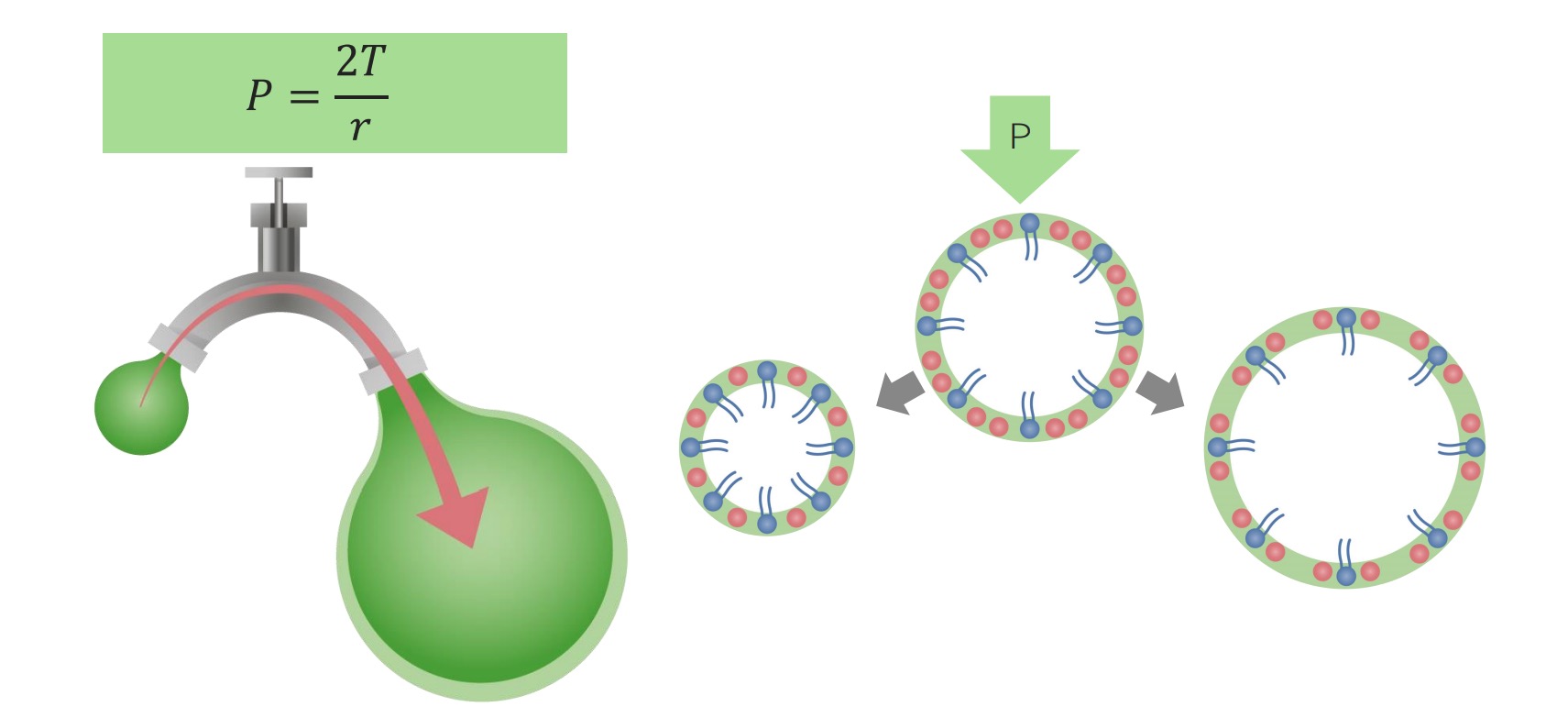
00:02 Acute hypoxia is where we are, and/or should I say acute hypoxemia. 00:07 Right, we always have to be a little bit more detailed. 00:09 It’s a V/Q mismatch, improves with supplemental oxygen. 00:14 So, this, for example, gives you examples such as pneumonia, COPD flares and PE. 00:20 Remember that no matter any time during a disease course of your lungs that supplemental oxygen is given, but you always have to utilize caution because of that condition that we called your hypoxic drive. 00:37 But, if it’s COPD flares, then you are left with really not much of an option. 00:44 Something that you want to keep in mind and something that you very much want to understand is the fact that what if your alveoli was to collapse. 00:52 This brings us to ALI, which stands for acute lung injury or we have acute respiratory distress syndrome. 01:00 What these have in common is the fact that ultimately, the alveoli collapse. 01:05 And when your alveoli collapse, they’re no longer functional. 01:09 This is called a pulmonary shunt. 01:11 A shunt means that there is deoxygenated blood passing in the systemic circulation. 01:17 You should be familiar with the right-to-left shunting in the heart that happens in cyanotic heart diseases, such as Tetralogy of Fallot. 01:24 So, why would you be so familiar with shunting in the heart and you’re not so familiar with the shunting in the lungs? The only way that you can get shunting of your blood from the pulmonary arterial side, which has normally a PO2 of approximately 40. 01:38 To get your PO2 of 40 to your pulmonary veins, you shunt across an alveoli that are no longer functional. 01:44 So, this is a intrapulmonary type of shunt. 01:48 Now, if there is an intrapulmonary type of shunt, if you were to give this patient oxygen, if that alveoli are collapsed, how should you get a significant response? You don’t get one. 01:59 Now, the same thing can also be applied to intracardiac shunt. 02:04 For example, say that you had a right-to-left shunt at some point in time. 02:08 If you did, then you get deoxygenated blood into your left side, from your right side. 02:14 So you’ve shunted your lung and thus by giving oxygen, are you having a response that you expect? No, you don't. 02:21 Look for that particular clinical description. 02:27 What else may cause acute hypoxemia? PaO2 or the partial pressure of oxygen inside the alveoli can become low as is the case at high elevations. 02:37 The reason for this is that the FiO2 or the fraction of oxygen in the air we breathe is effectively constant everywhere on the planet around 0.2. 02:46 What changes at high altitudes is the atmospheric pressure or barometric pressure. 02:51 As you remember, we find the partial pressure of oxygen by multiplying the barometric pressure which we normally consider to be 760 by the FiO2 which is 0.2. 03:02 At high altitudes, however, your alveoli see a lower partial pressure of oxygen because you're now multiplying a lower barometric pressure by the same 0.2 factor. 03:12 This then translates into decreased oxygen diffusion as the A-a gradient is decreased and ultimately results in hypoxemia and acute altitude sickness. 03:21 What else? Impaired diffusion. 03:23 Now things become a little bit easier. 03:24 What this basically means is the fact that you’re not able to properly cross your barrier. 03:29 What barrier? The barrier between the alveoli and trying to get your oxygen into your pulmonary capillary. 03:35 Impaired diffusion, couple of important points that we already discussed. 03:38 A-a gradient widened or normal, please? Good, widened. 03:43 What are some things that you wanna take in consideration for A-a gradient? The age is a big one, right? And the other big one is the fact that if you were to then increase your FiO2 in hospital setting. 03:55 Okay. 03:55 Now, the other big point to test is going to be DLCO. 04:01 Your DLCO laboratory examination with the impaired diffusion would find a decrease DLCO. 04:08 Hypoventilation can cause hypoxia, but this occurs with (and due to) hypercapnea. 04:14 So, hypoventilation, if there isn’t enough breathing, please understand that you’re having a decrease in oxygen, but that you also end up having an increase in carbon dioxide. 04:25 That’s not good. That displaces everything. 04:27 Acute respiratory failure is my issue. 04:29 We’ve walked through some important points of acute hypoxemia. 04:33 Let’s continue. 04:35 Now, the five possible physiologic causes of hypoxia. 04:38 Hypoxic respiratory failure is almost always caused by a V/Q imbalance or a shunt. 04:45 And by V/Q imbalance, we’re referring to something like perfusion defect, ventilation defect and dealing with a diffusion defect in general.
About the Lecture
The lecture Acute Hypoxemic by Carlo Raj, MD is from the course Respiratory Failures.
Included Quiz Questions
Which of the following is the least likely to respond well to supplemental oxygen?
- Acute lung injury
- Asthma
- Pulmonary embolism
- Acute exacerbation of COPD
- Pneumonia
Which of the following is NOT related to acute hypoxemia?
- Obesity hypoventilation syndrome
- V/Q mismatch
- Pulmonary shunt
- Impaired diffusion
- Acute hypoventilation
Which of the following can cause an intrapulmonary shunt?
- Atelectasis of lung
- Emphysema
- Asthma
- Pulmonary embolism
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Very Well Taught Lecture by Dr Raj, Very Easy to Understand
Why is he not speaking in full sentences? He's talking like Yoda I'm on my free trial and definitely won't be buying a subscription after this