Playlist
Show Playlist
Hide Playlist
Acute Back Pain
-
Slides AcuteBackPain AcuteCare.pdf
-
Download Lecture Overview
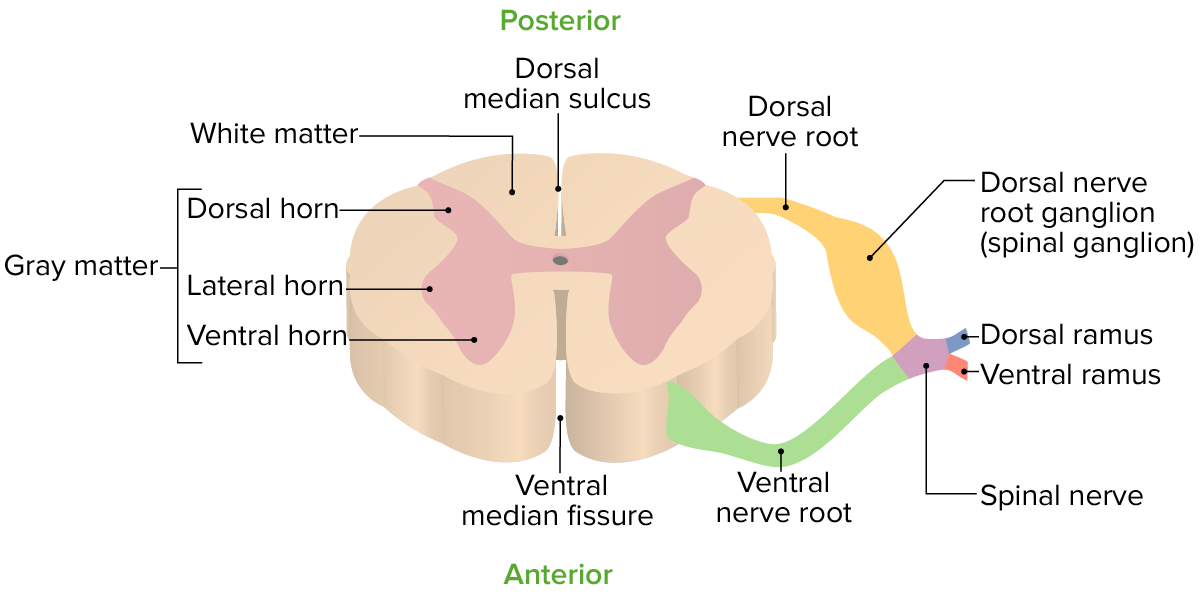
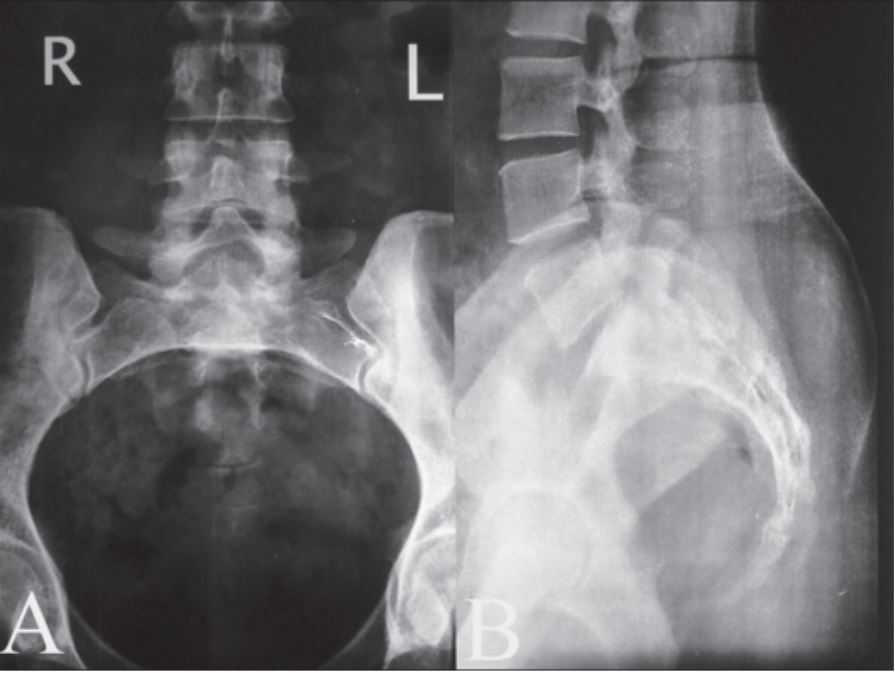
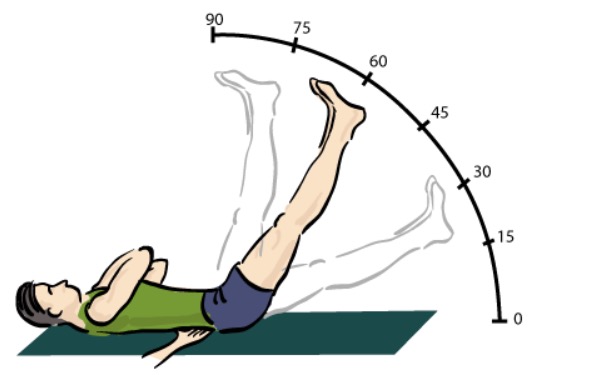
00:01 Alright. 00:02 Let's cover back pain today. 00:03 It's one of the more common things we see in primary care. 00:06 And I wouldn’t be surprised if a lot of you haven't suffered back pain at some point in your lives. 00:11 Let’s discuss it from an evidence-based perspective. 00:14 I’m going to start with a case. 00:15 I’ve got a construction worker coming in with back pain. 00:18 He is 35 years old, male. 00:20 He complains of back pain for the past five days. 00:23 He works in construction, was lifting a 50 kg bag when he felt acute pain in his lower back. 00:29 The pain has since improved, but he still has occasional radiculopathy that goes down his right leg. 00:35 No previous history of back injury. 00:38 So, what's the next best step in his care, just knowing that baseline history there. 00:43 Is it getting an MRI or plain radiographs? Is it just doing a physical examination and following up with analgesics? Or should we think about referring to an orthopedist? The answer is C, physical examination and analgesics alone. 00:57 Of course, you want to do a physical examination, but we’ll talk about how the natural history of most cases of back pain, even if it feels fairly severe at first and is associated with radiculopathy, still usually resolves within a couple of months. 01:13 So, overall, the point prevalence at any one time among adults, of back pain is 12% whereas the one-month prevalence is 23% and then 85% of patients in primary care have some kind of low back pain at some point in their lives. 01:31 And it’s oftentimes related to overuse and repetitive minor trauma, but we certainly see cases like this one as well where it was either due to an accident at work or motor vehicle accident or something more severe. 01:48 So, some key diagnoses to rule out, and think about when you see patients with low back pain specifically, include cauda equina syndrome. 01:56 Cauda equina is a back pain that’s also associated with specific neurological symptoms. 02:00 That include saddle anesthesia and the problems with bowel and bladder. 02:06 Now, that can mean a couple of things. 02:08 It can be - classically, it’s thought of as incontinence, but actually retention of stool and urine is more common in cauda equina syndrome than incontinence. 02:16 So, that’s something to think about. 02:17 The saddle anesthesia, though, has to be there to define cauda equina syndrome. 02:22 And because that's an acute compression of the nerve roots, it does require an emergent evaluation by a surgeon. 02:27 The other three diagnoses generally present with more persistent pain, more severe pain when you're talking about things like cancer, abscess and osteomyelitis, and particularly the latter two may be associated with more of a fever with abscess or osteomyelitis than you might see. 02:46 But in those cases that aren’t getting better, that aren’t following that natural course, thinking about these diagnoses can be helpful and then getting early imaging and follow-up. 02:56 But they are very rare. 02:58 Compared to the wide array of cases we see of back pain due to repetitive injury or minor trauma, cases of things like osteomyelitis or cancer are incredibly rare. 03:10 So, one of the questions is, well, what about imaging? Why not get started with x-rays? Why not start with MRI? And the question I would pose back is does that really change your management in most cases of low back pain? And in fact, in clinical studies, early imaging isn’t associated with a difference in clinical status at 12 months. 03:31 And then, you have to consider just how common changes, particularly the lumbar spine are as we get older. 03:38 So, by age 60 years, up to two-thirds of adults have evidence of disc herniation on MRI. 03:44 And about one in five has evidence of spinal stenosis. 03:47 So, it's the rare 60-year-old who has actually a normal MRI of the lumbar spine. 03:53 So, everybody has something. 03:55 But the fact is that those degenerative changes don't necessarily correlate well at all with the degree of pain and disability among patients. 04:03 So, therefore, that's - those are the limitations of imaging. 04:06 Like a lot of things in orthopedics with imaging, I really think about getting imaging when we’re going to do something about the pain and disability, such as concerning injection therapy or even surgery. 04:17 That's the time to order imaging, not at an early stage when you still want to give conservative management a good try.
About the Lecture
The lecture Acute Back Pain by Charles Vega, MD is from the course Acute Care.
Included Quiz Questions
A 72-year-old man with a past medical history of prostate cancer presents with 2 weeks of worsening low back pain and radiation of pain down his right leg. He does not have any fevers or chills. Upon examination, his straight-leg test is positive at 20 degrees, but his neurological exam is normal otherwise. Which of the following is the strongest indication for spinal imaging in this patient?
- History of prostate cancer
- Positive straight leg test
- Unilateral radiation of pain
- Back pain lasting > 10 days
- Age > 65
A previously healthy 40-year-old gardener presents to your office with 3 days of low back pain, which occurred suddenly after lifting a bag of compost. The pain has not improved. On physical examination, he has limited range of motion in the lower back and negative straight leg tests bilaterally. What is the next best step in management?
- Short-term analgesics
- Lumbar spine X-ray
- Lumbar spine magnetic resonance imaging
- Referral for spinal manipulation
- Bedrest
Which of the following diagnoses in a patient with low back pain does not require urgent care?
- Unilateral radiating pain
- Cauda equina syndrome
- Presence of metastatic cancer
- Epidural abscess
- Vertebral osteomyelitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |