Playlist
Show Playlist
Hide Playlist
Achalasia
-
Slides GD Esophagus.pdf
-
Download Lecture Overview
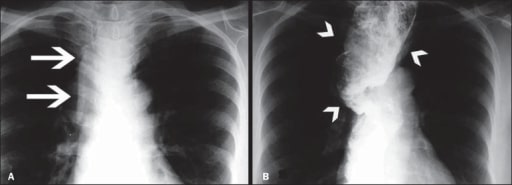
00:01 Move on to achalasia. 00:03 We’ve now, we’ve completed discussion of our infectious esophagitis, we did our reflux esophagitis and here, we’ll take a look at obstruction with achalasia of your lower esophageal sphincter. 00:19 It doesn’t wish to relax. 00:21 If you’ve lost ability to relax your lower esophageal sphincter… how? We’ll get into that. 00:26 There’ll be two major pathways. 00:28 One will be acquired, one will be genetic. 00:30 And you’ll like it. 00:32 And if that does… if the lower esophageal sphincter doesn’t wish to open, then what happens proximally in the esophagus? It’ll dilate. 00:39 And you know that you’ve heard of the term bird’s beak. 00:42 Now the bird’s beak would be the distal end of the esophagus that gives you like a beak, a smooth tapering. 00:48 But this, proximally, the head of the bird, we need to say, ‘with the dilation part’. 00:55 It’s a proximal dilation and you have the smooth tapering, upon your barium swallow. 01:02 Functional obstruction of LES causes dysphagia to both, to both solids and liquids at the same time. 01:10 Endoscopy, not a good test for diagnosis because you can’t really see the issue with the lower esophageal sphincter and so that’s kind of different from really, any other type of pathology that we’ve seen in the esophagus. 01:24 Endoscopy has been quite a bit of the definitive diagnosis or the definitive tool, tool for diagnosis. 01:32 Dealing with esophageal cancers, dealing with strictures, and so on and so forth. 01:37 So therefore here, you’re going to be doing a pressure test. 01:41 Take a look at the cartoon on the left. 01:44 The cartoon on the left is literally showing you the diaphragm there, but then the lower esophageal sphincter which does not want to open. 01:53 And so therefore with that increased constriction or lack of relaxation of lower esophageal sphincter; if you take a look at the imaging study on your right, you’ll notice this same cartoon on your left is manifested on the right as being the bird’s head with proximal dilation and notice at the very end here, on the bottom right, there’s smooth tapering, in other words your bird’s beak. 02:17 This is achalasia. 02:19 Do not confuse this with reflux. 02:22 Could there be reflux associated with this? Sure, but my goodness, not as extensive as what you would find with GERD. 02:28 Here the problem is, the lower esophageal sphincter doesn’t want to relax. 02:32 Now, let’s talk about why your lower esophageal sphincter doesn’t wish to relax. 02:39 Give me some peptides that you know of that are responsible for normal relaxation physiologically of the LES. 02:45 Nitric oxide, maybe VIP - Vasoactive Intestinal Peptide, and nitric oxide. 02:52 What if these were absent in your patient? Well, gone is the relaxation of LES, welcome to achalasia. 03:01 The chest X-ray may show a fluid level in the chest with absent gastric bubble. 03:06 Why? Because you can’t even get anything in there. 03:09 The lower esophageal sphincter doesn’t wish to relax. 03:13 So what is the confirmatory test for achalasia? It is not endoscopy. 03:20 Remember, you are going to do an EGD to rule out important causes perhaps, right? The esophagogastroduodenoscopy. 03:29 However, the manometry measures the pressure within the esophagus. 03:36 Let’s begin. 03:38 In the upper portion of your esophagus, when you eat a bolus or consume a bolus, it enters esophagus. 03:44 What then happens with pressure? Increases. 03:48 What should happen physiologically down the lower esophageal sphincter? It should relax. It’s called receptive relaxation. 03:58 In achalasia, the lower esophageal sphincter does not relax. 04:03 That’s your problem, increased pressure. 04:07 Esophagogastroduodenoscopy necessary to rule out EGD is necessary to rule out achalasia due to secondary causes such as gastric cancer cardia or perhaps even Chagas disease. 04:21 So you need to make sure that you get in there and rule out other issues, ecause your patient is going to be complaining of dysphagia to solids and liquids, non-progressive. 04:33 Cancer is important for you to rule out. 04:35 My goodness! Chagas could in fact cause achalasia. 04:40 Now what Chagas means is the following; you’re taking a cruise - I’m being silly here but this will help. 04:47 You’re taking a cruise down to South America. 04:53 You end up acquiring an infection known as Trypanosoma Cruzi. 05:02 South America, Trypanosoma Cruzi, resulting in Chagas disease. 05:07 Chagas disease for you, and I keep repeating this, will be responsible for 3 major sites for pathology. 05:17 One would be the esophagus with achalasia, dilation of the proximal esophagus. 05:25 Chagas with amastigotes in the heart destroying the myocardium, resulting in dilated cardiomyopathy. 05:34 Chagas disease down in the intestine. 05:38 Trypanosoma Cruzi resulting in toxic megacolon. 05:44 Dilation, dilation, dilation. Chagas, Chagas, Chagas. Chagas, Chagas, Chagas. 05:50 Three different locations big time that you want to pay attention to are Chagas, Trypanosoma Cruzi, what was the amastigote that I told you about? In microbiology, you should know the amastigote phase for some of these organisms, because this is what they’re going to give you. 06:06 They’ll give you a picture of amastigotes in the myocardium, and you should be... 06:11 you should know that is what it is, resulting in a dilated type of cardiomyopathy. 06:16 Endoscopic pneumatic dilation would be perhaps necessary but management here and risk, very possibility that you may dilate your esophagus too much resulting in rupture; number one. 06:33 Number 1. 06:34 Number 2, with management, another option would be actually to inject botulinum. 06:42 You know about botox, amazing. 06:47 But point is, people are actually injecting this so that they can then inhibit the release of acetylcholine from the neuromuscular junction to get away, or to remove the wrinkles. 06:56 Right, botox. 06:57 Well, same concept, but now where are you? The esophagus, causing well, hopefully maybe perhaps to assist with relief and to bring about relaxation. 07:09 There’s something called the Heller myotomy, a myotomy. 07:13 Then now at this point, you’re thinking about maybe, maybe relaxing the lower esophageal sphincter by literally removing parts of the muscle - a myotomy. 07:24 Also keep in mind that you have calcium channel blockers for antagonist. 07:28 And PPIs are useful adjuncts to therapy as well. 07:32 Adjuncts because you’re trying to, number one, create relaxation and at the same time remember, any type of lesion down by the distal esophagus, you’re always worried about reflux. 07:44 So PPIs become an important adjunct therapy.
About the Lecture
The lecture Achalasia by Carlo Raj, MD is from the course Esophageal Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is a confirmatory test for achalasia?
- Manometry
- Chest X-ray
- Endoscopy
- Chest CT scan
- Abdominal ultrasound scan
Which of the following is the main mechanism of symptom development in achalasia?
- Failure of the LES to relax
- Failure of the LES to contract
- Loss of peristalsis in the proximal esophagus
- Increased peristalsis in the distal esophagus
- Atrophy of the LES
Which of the following reflects the appearance of achalasia on barium swallow?
- Bird beak
- Corkscrew
- Shouldering sign
- Finger-in-glove sign
- Knuckle sign
Which of the following is the definitive therapy for achalasia?
- Heller myotomy
- Proton pump inhibitors
- Botulinum toxin
- Calcium-channel blockers
- Endoscopic pneumatic dilation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |