Playlist
Show Playlist
Hide Playlist
Abdominal Pain: Cases
-
Slides AbdominalPainCases AcuteCare.pdf
-
Download Lecture Overview
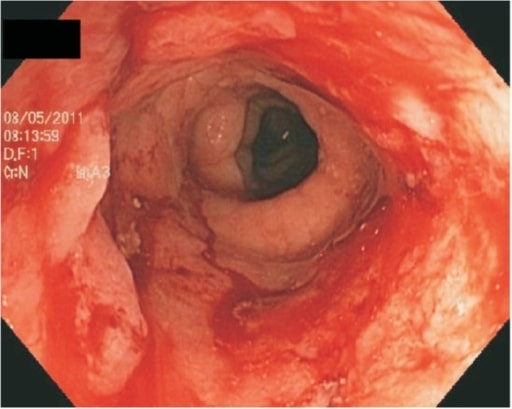
00:01 All right. 00:02 So, we’ve discussed the principles behind abdominal pain and its workup previously. 00:07 Now, we’re going to talk about cases to try to drive those points home. 00:11 So, we’re going to start. We have a few to get through. 00:14 And definitely think as you – as we move through these, what you would do and there's some questions. 00:19 Feel free to pause any time if you want to really think through the case. 00:23 So, we’re going to start with central abdominal pain. 00:25 I’ve got a 45-year-old woman. 00:27 She has a one-month history of central abdominal pain. 00:29 It’s worse with food and it’s cramping in nature. 00:31 That's the history we’ve got. 00:34 We also know that it does not radiate and it can promote mild nausea when it’s severe. 00:39 So, based on what we discussed regarding principles and getting a good history in particular, which of the following questions will be the highest yield to further evaluate this patient? A, do you have any blood in your stool? B, do you have a family history of inflammatory bowel disorders? C, tell me about surgeries that you’ve had. 00:57 Or D, do you have any pain – do you have pain over your spine as well? So, we have a one-month history of central abdominal pain. 01:05 It could be upper or lower GI. 01:07 It’s worse with food and cramping in nature. 01:09 That’s kind of hard to really give much of a differential, but doesn't radiate and she has some mild nausea, which – that could be just related to the pain. 01:17 To me, these questions are all legitimate questions. 01:22 The one that sticks out to me is, if she has had a surgery, this is kind of vague abdominal pain is pretty common after a major bowel surgery. 01:32 Maybe she had a bleeding ulcer that had to go through repair. 01:36 She had a history of complicated pancreatitis, or whatever it may be, if she has a history of abdominal surgery or surgeries, that's going to give me some light that maybe this is related to some kind of postsurgical influence and complication. 01:50 Maybe it's a partial small bowel obstruction or maybe it's just adhesions within her abdominal cavity that’s promoting the pain. 01:58 The other questions are certainly legitimate, but not as high a yield as talking about previous surgeries. 02:07 So, I thought her pain sounded a little bit more upper GI in nature. 02:11 Maybe it's more of an acid-related disorder. 02:15 I did mention how biliary colic can be epigastric. 02:18 And so, the other things to ask that, I think, are particularly impactful when you have an upper gastrointestinal disorder, many patients have tried antacids, many have tried over-the-counter proton pump inhibitors. 02:32 If it did not get better after taking a proton pump inhibitor for a week, say, at least improve a little bit, it's probably not an acid-related disorder in my opinion. 02:43 It’s time to look elsewhere. 02:44 Think about biliary colic, pancreatitis, some of the other things that cause upper GI problems. 02:50 And then think about the patient's risk factors for acid-related disorders versus cholelithiasis because they are different. 03:00 For acid-related disorders, using lots of caffeine, using lots of alcohol, smoking, previous history of acid-related disorders. 03:08 Cholelithiasis, overweight and obese, female, 40 years old, those things can be telling as well. 03:17 All right. Let’s move on to case number two. 03:19 Now, we’re talking about inferior abdominal pain. 03:22 A 25-year-old woman presents with persistent inferior abdominal pain over three weeks. 03:26 It has been associated with several episodes of hematochezia or blood in the stool, gross red blood. 03:33 The pain is a dull ache. 03:35 She has fatigue and occasional tactile fever. 03:38 So, this is definitely, with that short history, giving me a strong inclination as to what the patient actually has. 03:45 And so, what should you consider regarding this case? A bleeding peptic ulcer is likely given her age. 03:52 A rectal examination should not be performed. 03:54 A trial of proton pump inhibitors with reevaluation in two weeks is warranted. 03:59 She needs immediate laboratory work and probable colonoscopy. 04:03 And it’s D because I'm really worried about this patient and the particular risk for inflammatory bowel disease. 04:10 Let’s go through some explanation on this case. 04:14 So, first of all, it sounds like a lower GI problem. 04:17 She's having – the pain is lower in her abdomen and she has hematochezia as well. 04:22 Remember, bleeding from an ulcer would often present as melena, not bright red blood. It would look black, not red. 04:30 Yet hematochezia, oftentimes it’s concerning always, and we have to include terrible things like inflammatory bowel disease and malignancy on a differential, but usually it's due to very simple disorders such as hemorrhoids or fissures, but those things, of course, aren't associated with abdominal pain. 04:47 So, therefore, if you have the two, abdominal pain with hematochezia, it’s more ominous than either alone. 04:53 And then the fact that she has some fever, she's only 25 years old, it all does point towards inflammatory bowel disease. 05:00 So, when I talk about needing a laboratory workup, she needs a CBC as well as some measure of inflammation and there are some specific serologic markers for both Crohn's disease and ulcerative colitis, but she needs to be referred to GI promptly and urgently, so she can get a colonoscopy with biopsy. 05:19 That's going to be diagnostic for her. 05:21 And then she can be put on disease modifying therapy, important in cases of inflammatory bowel disease. 05:27 If she has something more rare, an arteriovenous malformation, cancer, it’d be very rare in a woman who doesn’t have a strong family history of colorectal cancer to develop cancer, but that's what colonoscopy is for as well. It will diagnose those conditions as well. 05:44 Okay. Let's look at cramping and intermittent abdominal pain now. 05:48 So, I’ve got a 40-year-old female, complains of inferior abdominal pain for two weeks. 05:52 It’s cramping and intermittent. 05:55 It's worse with activity and unchanged with food. 05:59 She has some mild dysuria and constipation. 06:02 She's had menorrhagia with her last two menses. 06:04 So, she's 40 years old and has actually a variety of different symptoms in addition to her abdominal pain. 06:11 And so, which of the following batteries of test is most appropriate? Urinalysis? Urine pregnancy test? Pelvic examination? How about a CBC, a sed rate, and a CT of the abdomen? Or a faecal occult blood colonoscopy, CBC, or a pelvic examination followed by a CT of the abdomen? Which is the most appropriate in this case for initial analysis? It’s this one. 06:35 So, I think – let's discuss the case a little bit and we’ll go through it. 06:41 So, she does have multiple potential causes for her pain. 06:44 This could very well be a non-GI cause of abdominal pain. 06:50 And that's why it's important to perform the simplest and do the basics first. 06:55 And that means – and this is one of my pearls, is whenever there is the remotest possibility of pregnancy, even in patients with a tubal ligation in their history, getting urine pregnancy test is very low cost, but it can be incredibly high yield when it’s positive. 07:12 And what you don't want to do is start sending the patient down a road of potentially getting a CAT scan or other testing which could harm a potential fetus without knowing that she's not pregnant. 07:23 So, she's only 40. Definitely worth a pregnancy test. 07:26 In this case, urinalysis as well. 07:28 Simple test to do. It can help with the potential for a UTI. 07:32 She did have some dysuria. 07:34 Or a kidney stone. This could also be a kidney stone. 07:37 And sensitivity is not nearly 100%, but again, in office, you get results in minutes and it can be high-yield. 07:43 If there's a lot of blood that returns on the urinalysis and the lady is not having her menses at this time, certainly makes you think that this is going to be a genitourinary disorder. 07:55 And then finally, I’ll always do a pelvic examination for low abdominal pain when there is no clear-cut diagnosis. 08:02 But in general, it's a good idea at least to do a bimanual examination. 08:06 In this case, an ultrasound of the pelvis may be helpful for the possibilities of endometriosis and uterine fibroids. 08:14 And a CT is going to be less diagnostic for those conditions. 08:19 So, start with an ultrasound. 08:22 All right. 08:23 So, those three cases, I think, emphasize some the points on upper, lower and non-GI sources of pain. 08:30 And hopefully, that helps you in your clinical acumen. 08:34 I'm sure you will see cases of abdominal pain and the differential featured on your examination. 08:40 And you'll see questions just like the ones I just posed to you and you should feel better prepared to answer them. 08:46 Thanks.
About the Lecture
The lecture Abdominal Pain: Cases by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Woman with Central Abdominal Pain
- Woman with Inferior Abdominal Pain
- Cramping and Intermitten Abdominal Pain
Included Quiz Questions
Which of the following is NOT a risk factor for gallstones?
- Caffeine consumption
- Obesity
- Female sex
- Age
- Hypertriglyceridemia
A 22-year-old man presents with weight loss and bloody diarrhea for 2 months. Which of the following is the most likely diagnosis?
- Inflammatory bowel disease
- Bacterial gastroenteritis
- Viral gastroenteritis
- Chronic pancreatitis
- Peptic ulcer
Which of the following confirms a clinical diagnosis of ulcerative colitis?
- Colonoscopy and biopsy
- Upper endoscopy and biopsy
- Barrium swallow
- Contrast-enhanced computed tomography scan of the abdomen and pelvis
- Abdominal ultrasound
Which of the following conditions is most likely in an adult with a history of abdominal surgery who presents with chronic postprandial abdominal discomfort and occasional nausea with abdominal distention and tympany?
- Partial small bowel obstruction
- Pancreatic cancer
- Abuse of nonsteroidal anti-inflammatory drugs
- Inflammatory bowel disease
- Cirrhosis
A 29-year-old woman presents with 1 week of intermittent lower abdominal cramping without any diarrhea or constipation. She reports some mild nausea without vomiting. She has missed her last episode of menstrual bleeding. She has a history of pelvic inflammatory disease, but does not have abnormal vaginal discharge or dysuria at the moment. Which of the following tests is most appropriate at this point?
- Serum beta hCG
- Pelvic computed tomography scan
- Pelvic ultrasound
- Urinanalysis
- Complete blood count
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |