Playlist
Show Playlist
Hide Playlist
Wilson Disease
-
Slides GIP Wilson Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
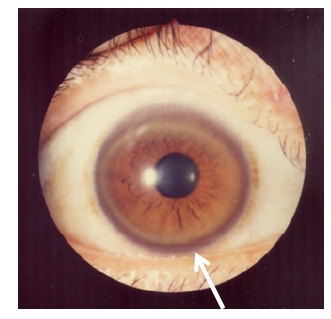
00:01 Welcome! With this talk, we're going to cover Wilson's disease. 00:05 And like all the eponymous diseases named after a patient or a doctor, and unless you remember what it's about, it and doesn't help you in terms of the name. 00:13 But after this talk, you will hopefully remember that Wilson's disease is an autosomal recessive disorder. 00:19 It's characterized by copper accumulation in a variety of organs, and mostly liver and brain and cornea. 00:25 And since clearly, this is a talk that's in the GI pathophysiology series of talks. 00:31 We're going to emphasize what goes on in the liver. 00:33 But we'll look at some of those other organs as well. 00:37 The epidemiology of this, it's a relatively rare entity, but one you should be aware of about one per 30,000 live births. 00:46 Because of the copper accumulation, patients who are going to be symptomatic, tend to present relatively early in life. 00:53 And so it can be in the pediatric population or in young adulthood. 00:59 The pathophysiology, the problem with this disease, is we have lost a copper transporting protein. 01:07 The gene itself is indicated there ATP7B, it's an ATPase, it's on chromosome 13. 01:13 Do not memorize that. 01:15 Just know that the necessary or the important protein in this is a copper exporter, it will allow the hepatocytes to get rid of excess copper. 01:26 So what's the normal pathway of copper absorption within the GI tract? So copper like iron is absorbed in the duodenum and ileum. 01:34 And here we have absorbed and going through the portal circulation to the liver, where it is taken up by specific ATPase is taken up by the hepatocytes. 01:45 Hepatocyes will use it for a variety of things. 01:47 It's important as unnecessary cofactor in electron transport, and superoxide dismutase activity and in matrix crosslinking. 01:56 It's also important that we get rid of the excess. 02:01 So you don't want a lot of the city around because it will generate oxygen free radicals which will cause damage to the hepatocytes. 02:11 So any excess copper is excreted through the bile and then ends up going away in the stool. 02:19 So if we cannot excrete the excess copper, due to the mutations in the transporter, we'll get accumulation of the copper and the hepatocytes will undergo apoptosis. 02:34 We can see similar excess accumulations of copper and a variety of other tissues, which will lead to injury. 02:40 And the more common areas where we will see pathology or in the brain and in the eye. 02:46 And in the kidney. 02:48 The clinical presentation for Wilson's disease. 02:51 So the liver disease, which is going to be probably our earliest manifestation that's going to be anything that you can expect going wrong with the liver leading to hepatomegaly. 03:03 An accumulation of the copper, but eventually with ongoing apoptosis, this is going to progress to cirrhosis. 03:11 And then everything we've talked about when we talk about cirrhosis. 03:14 So go back to that other talk in the series when we talk about cirrhosis. 03:19 And you'll remember everything that's on this list. 03:22 The neurologic symptoms occur because the neurons in the basal ganglia and the associated parenchymal cells, astrocytes etc. 03:32 In the basal ganglia, the cerebellum and the cerebrum accumulate excess copper, which leads to defects in the normal activity of these neurons. 03:42 In the basal ganglia, we will have defects that are associated with tremor, or with movement disorder. 03:49 And that's what the basal ganglia are responsible for. 03:52 In the cerebellum while we get dysarthria. 03:54 So the - not being able to speak appropriately, dysarthria. 03:58 You may also get dysphasia in coordination and inability to walk or ataxia. 04:04 In the cerebrum, you may actually have psychosis and dementia. 04:08 There will be hemolytic disease. 04:11 It's a Coombs-negative, so there's no antibody associated hemolytic anemia, and this will exacerbate the liver jaundice because we're getting breakdown or hemolysis of red cells. 04:22 This is happening because of excess levels of circulating amounts of copper that copper is accumulated within the erythrocytes probably leading to instability of the plasma membrane of the cells, but also leading to increased rates of oxidation of hemoglobin, and also with inhibition of the pentose monophosphate shunt, for example. 04:47 So that the erythrocytes don't have their normal capacity to maintain their architecture. 04:53 That Hemolytic Anemia is commonly seen with acute liver failure in Wilson's disease. 04:59 A characteristic finding on clinical examination is the Kayser-Fleischer ring. 05:04 This is a copper deposition in decimates membrane, in the cornea, and it will be present in almost all patients who have neurologic or psychiatric presentations. 05:14 And if you just have hepatic disease, roughly 50% of patients will have this, but it's an easy marker to see. 05:21 How are we going to make the diagnosis? So it's a physical examination in a juvenile who is presenting with signs of liver failure with or without the central nervous system manifestations. 05:32 We will do a slit lamp examination looking for the Kayser-Fleischer ring. 05:37 And then we will do additional laboratory workup. 05:41 So with hepatocyte injury due to the excessive accumulation of the copper, we will see elevated transaminitis. 05:49 Characteristically the AST to ALT ratio is greater than 2. 05:53 Personally, I can never remember that. 05:55 And it's nonspecific. 05:57 So I would just say there's elevated transaminitis. 06:00 There will be decreased serum ceruloplasmin. 06:02 So ceruloplasmin is the normal circulating protein that binds up copper, and also can carry it out of the bloodstream. 06:11 With elevated levels of copper, more, the ceruloplasmin is binding, and that level goes down. 06:17 Now it's also synthesized by the liver and as we get progressive liver damage will make less of the protein as well. 06:23 But that decrease ceruloplasmin is actually a pretty good marker for too much circulating copper. 06:29 We can also look for copper being excreted in the kidneys, so we can actually do a 24 hour urine sampling and measure that. 06:37 And a complete blood count. 06:39 And mainly we're looking for signs of hemolytic anemia. 06:44 Imaging, we can do an ultrasound and look for cirrhosis, but that's really kind of too far along. 06:50 We want to actually prevent cirrhosis. 06:53 So the gold standard test once you've documented that you have low ceruloplasmin. 06:57 And you've had elevated levels of circulating copper, particularly in a 24 hour urine sampling. 07:02 We're going to do a liver biopsy. 07:04 And we're going to see increased copper detected by quantitative assays. 07:08 We can then also do the specific molecular genetic analysis looking for mutations in the transporter ATPase. 07:15 How are we going to manage these patients? Let's cut the copper up. 07:19 So no more eating pennies. 07:21 No, that's not the way you do it. 07:22 But there are a lot of foods that are relatively rich in copper, so you reduce that. 07:28 Any excess copper that is in the circulation, you can administer drugs that kill it and allow you to urinate it away. 07:36 If it's poorly tolerated to take penicillimine or others, you can do oral zinc, which in many ways will help with the excretion of the copper. 07:44 And in for very severe cases, because we're lacking the necessary enzyme. 07:50 We'll give them a brand new liver to start over with. 07:53 And that may be all that you can do once you have in stage cirrhosis. 07:58 With that, we will talk about prognosis. 08:01 So five year median survival after the parents have neurologic symptoms. 08:05 That's not great. 08:06 But if we're able to manage and reduce the levels of copper overall, they can do quite well. 08:14 95% of patients who develop acute liver failure will die within days without liver transplantation. 08:23 As I was intimating in the previous slide, survival with appropriate treatment is excellent. 08:27 Even in the presence of liver damage, we just have to minimize further accumulation of more injury to the liver. 08:35 We'll conclude here with a little bit about copper metabolism and Wilson's disease.
About the Lecture
The lecture Wilson Disease by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
In what age range do patients with Wilson disease typically become symptomatic?
- 5–35 years old
- 35–75 years old
- 75–90 years old
- 1–5 years old
- Before 1 year old
Which of the following molecules is defective in Wilson disease?
- Specific ATPase
- Ceruloplasmin
- Hemochromin
- Ferritin
- Beta-galactosidase
What is NOT a common finding in Wilson disease?
- Tinnitus
- Hepatomegaly
- Cirrhosis
- Wing-flapping tremor
- Dysarthria
Which of the following findings is consistent with Wilson disease?
- Kayser-Fleischer rings
- Central retinal artery occlusion
- Retinopathy
- Bitemporal hemianopia
- Lymphedema
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |