Playlist
Show Playlist
Hide Playlist
Narrow Complex Tachycardias
-
Emergency Medicine Tachyarrhythmia.pdf
-
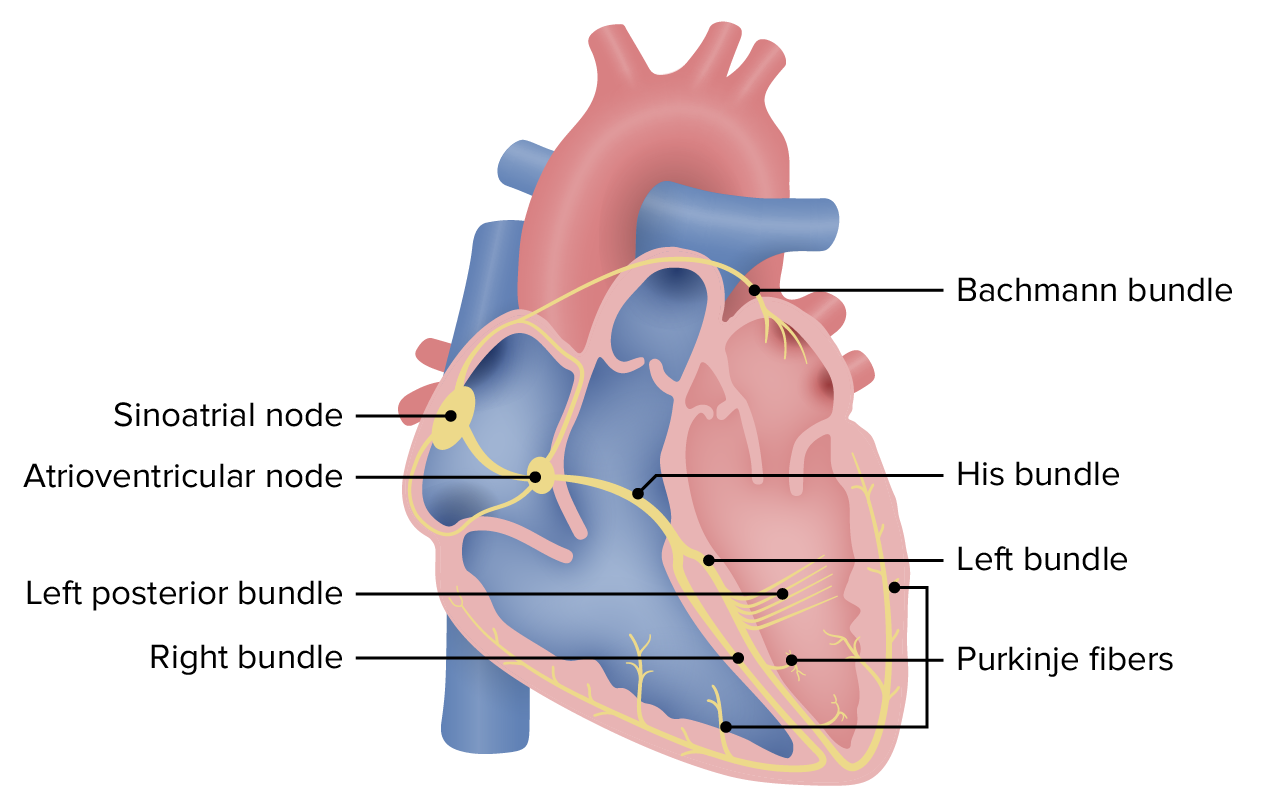
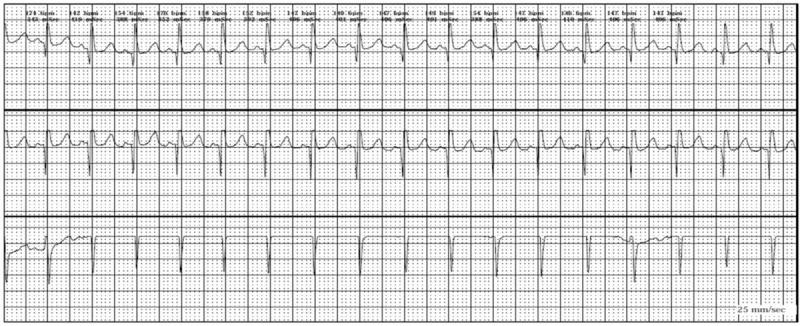
Download Lecture Overview
00:01 Alright, so we covered our wide complex rhythms. 00:05 Again, wide complex rhythm, we're gonna treat it like ventricular tachycardia and we're gonna be safe. 00:13 Now we're gonna move on to narrow complex rhythms. 00:16 So narrow complexes suggests a supraventricular origin of the rhythm. 00:20 All narrow complex rhythms must by definition originate above the AV node because they're using those fast conduction pathway in the His-Purkenji system. 00:31 There are several different loci from which narrow complex dysrhythmias can originate. 00:36 There's of course the Sino-Atrial node which is where sinus tachycardia comes from, there's atrial rhythms like atrial fibrillation, atrial flutter, multifocal atrial tachycardia, etc. 00:48 And then there are ectopic foci of pacemaking which are gonna be your supraventricular tachycardias. 00:56 Once you've identified that you have a narrow complex tachydysrhythmia, like we said before your next question is, is it regular or irregular? So we're gonna start off talking about the irregular rhythms. 01:09 So our two irregular rhythms are atrial fibrillation and atrial flutter. 01:14 In atrial fibrillation what's happening is electricity is wheezing around the atria in a completely uncontrolled way so the conduction in the atria is random, it’s unpredictable and impulses are sent down through the AV node from the atria in random intervals. 01:32 So basically anytime the node is not refractory an impulse might be sent to it and would then be conducted to the ventricles. 01:40 This produces the classic irregularly irregular rhythm of atrial fibrillation, the electrical conduction in the atria is random, the transmission of the impulses to the AV node is random and that produces a rhythm that has no regularity whatsoever in terms of the R-R interval. 02:01 Atrial flutter by contrast is a little bit more organized. 02:05 When the atrial flutter, they typically conduct at a regular rate of 300 atrial beats per minute. 02:12 This produces what is usually a regular ventricular response rate. 02:18 Now the ventricles typically cannot conduct at 300 beats per minute so the most common ventricular rate we see in atrial flutter is gonna be 150 so two to one conduction every other atrial beat gets conducted to the ventricles so the atrial rate is 300 the ventricular rate is 150. 02:39 However you can get an irregular rhythm with atrial flutter because you can sometimes get variable conduction through the AV node. 02:48 So let’s talk about how you diagnose atrial fibrillation. 02:52 So like we said before the QRS complexes are narrow so there are less than a 120 milliseconds long. 02:58 The rate or the RR interval is irregularly irregular so I've denoted the RR interval for several of the beats on this rhythm strip and you can see that one is 7, one is 15, one is 10, one’s 8, one’s 10. 03:13 There's no predictability to it they are just randomly fluctuating in terms of how frequently the QRS’s are coming along. 03:21 There's also a randomly fluctuating baseline so you can see there's that waviness in the baseline that represents the fibrillatory action of the atria and there are no organized P waves so you're not seeing regular organized atrial activity. 03:38 You're just seeing this random fluctuation on the baseline. 03:42 Now by contrast, atrial flutter looks a little bit different. 03:46 In atrial flutter you have the saw tooth atrial waves and so I sort of outlined those for you in green but you can see they go up and down almost like a teeth of a cross cut saw. 03:55 Like we said before, the most common atrial rate in atrial flutter is gonna be 300 beats per minute and I've marked all of the atrial waves with arrows so that you can see where they are. 04:07 The ventricles can't conduct at 300 beats per minute so every other atrial beat is conducted to the ventricles producing a QRS rate of 150 and you can see the QRS complexes noted again on this rhythm strip. 04:24 This produces a two to one atrial to ventricular conduction rate so I've highlighted each set of two atrial waves with the one corresponding ventricular wave and you can see, you've got two atrial waves one ventricular wave; two atrial waves one ventricular wave, so this is a two to one atrio-ventricular conduction ratio. 04:45 Now, that’s not always what we see, you can see flutter with slower ventricular response rate so in this particular ECG, we're seeing a four to one conduction ratio so for every four atrial waves we have a QRS complex but you can also see 3 to 1, 5 to 1 and variable conduction rates that produce an irregular QRS interval. 05:11 How do we manage atrial fibrillation and atrial flutter? First and foremost, if your patient is unstable your cardiovert them cuz that’s what you do for every single unstable tachyarrhythmia, but assuming they're stable, we're gonna be using AV nodal blockers to try to decrease the ventricular response rate, so the goal is not to get the patient out of atrial fibrillation or flutter but the goal is to slow down the heart rate by decreasing the ventricular response rate. 05:42 So you block the AV node, you make it more difficult for impulses from the atria to pass through into the ventricles and you slow down the ventricular rate. 05:52 Again calcium channel blockers or beta blockers are the mainstay of treatment for this. 05:57 Amiodarone can also be used and is appropriate in some circumstances. 06:02 It has AV nodal blocking effects as well as global antidysrhythmic effects. 06:07 I do wanna mention that AFib is commonly associated with underlying noncardiac pathologies. 06:15 So for example, patients with sepsis, patients with intra-abdominal catastrophes, patients with pulmonary emboli, they will often present an atrial fibrillation and if AFib is a complication of some other underlying disease process it’s usually safest to focus your treatment on that underlying disease process rather than focusing on rate control or slowing down the atrial fibrillation. 06:46 There's actually some studies that show worse outcomes when we treat AFib aggressively particularly in patients with sepsis as oppose to when we just leave it alone and focus on the sepsis. 06:59 So if you think that your AFib is related to some underlying disease process, you might consider withholding specific rate control agents but if the patient’s coming in with this as their primary complaint, then of course you're gonna wanna treat it. 07:14 Alright, so the other thing that we wanna think about with atrial fibrillation is anticoagulation. 07:19 Not every patient with AFib needs to be anticoagulated, but there are some indications for anticoagulation that you wanna think about. 07:28 So any patient with a prosthetic valve is always gonna be anticoagulated. 07:32 Honestly, whether they are or aren’t in AFib. 07:34 A patient with a prior history of stroke or TIA should definitely be anticoagulated if they're in AFib, and then there's a scoring system called CHADS2 and I put it here on the slide, I'm not gonna go through it in any kind of detail but I want you to be aware that there is this scoring system that helps us assess the risk of stroke related to atrial fibrillation and if your patient has a CHADS2 score of equal or greater than two, you wanna think about anticoagulating them assuming that there aren’t any contraindications.
About the Lecture
The lecture Narrow Complex Tachycardias by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock.
Included Quiz Questions
Which of the following statements regarding irregular rhythms is INCORRECT?
- Atrial fibrillation is described as a rapid regular rhythm
- Conduction through the atria is random and unpredictable in atrial fibrillation
- Atria conduct at a regular rate in atrial flutter
- The rhythm is usually regular in atrial flutter
- Impulses are sent to AV node at random intervals in atrial fibrillation
Which of the following is NOT a finding in atrial fibrillation?
- Sawtooth atrial waves
- Narrow QRS
- Irregularly irregular ventricular rate
- Randomly fluctuating baseline
- No organized P-waves
Which of the following is typically NOT an appropriate management for atrial fibrillation/atrial flutter?
- Spironolactone
- Cardioversion if unstable
- Rate control with a calcium channel blocker or beta blocker
- Treatment of underlying disease if noncardiac pathology is present
Which of the following statements regarding anticoagulation in atrial fibrillation is correct?
- Patients with mechanical prosthetic valves will require anticoagulation.
- Every patient needs anticoagulation.
- Anticoagulants are contraindicated in patients with prior stroke/TIA.
- A CHA2DS2-VASc score of 2 or more means the patient should not receive anticoagulation.
- The CHA2DS2-VASc score measures the risk of myocardial infarction associated with atrial fibrillation.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
simplified ,high yield content , Dr Juliana has charisma draws the audience attention