Playlist
Show Playlist
Hide Playlist
Vagus Nerve
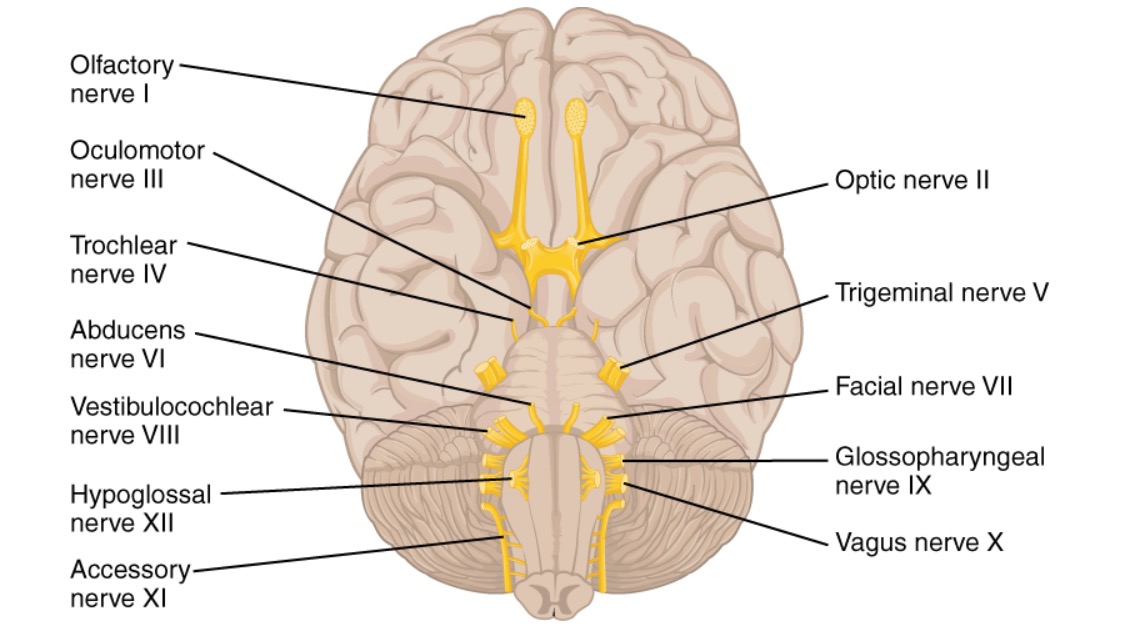
00:00 Vagus. Vagus is the 10th cranial nerve, comes out through the jugular foramen, lies within the carotid sheath. It’s so close to the midline, it runs in front of the subclavian artery. 00:18 So far, so good. Now that distinguish the difference between the right and the left vagus. On the right vagus, as it passes in front of the subclavian, the recurrent laryngeal nerve is given out which hooks around the subclavian and comes back. That’s your recurrent laryngeal nerve. On the left side, it goes down to the arch of aorta, then it hooks back and then you have ligamentum arteriosum. 00:50 To the left of ligamentum arteriosum it hooks and comes back to the neck. So on the right side it is hooking back on the subclavian artery, on the left side it’s hooking back on the arch of aorta. So the action of the vagus and the glossopharyngeal are quite similar in the pharynx and the larynx and superiorly. 01:22 What are the main branches of the vagus? Just tell me some main branches you can think of. 01:25 Recurrent laryngeal you said, that’s fine. Anything else? Is it the external laryngeal? External laryngeal. 01:37 Is that a branch of the vagus? That’s right. Though you have, you are right, because you said that. Vagus gives off a superior laryngeal nerve which divides into an external laryngeal and an internal laryngeal, and then you have the recurrent laryngeal coming down. So because, this essentially supplies the whole of larynx. So your superior laryngeal nerve divides into external laryngeal and internal laryngeal. The external laryngeal nerve supplies the cricothyroid. All the other motor muscles in the larynx are supplied by the recurrent laryngeal. The action of cricothyroid is for high pitched voice. So if a patient has got a superior laryngeal nerve injury or an external laryngeal nerve injury, they will have absence of high pitched voice. But if the recurrent laryngeal nerve is affected, what happens? Lost voice. One side stutters. 02:40 What if one side is divided, what is it? Hoarseness. Bilateral? Stridor or aphonia. Completely, there’s probably no speech at all. Sensation, above the vocal cords is supplied by the internal laryngeal nerve, below the vocal cord is supplied by the recurrent laryngeal. 03:08 So similar to your tongue, if you divide it into -- Does it abduct the vocal cords as well? Abduction of the vocal cords as well. 03:16 Was that the recurrent laryngeal or was that the superior laryngeal one? Ah, recurrent laryngeal because superior laryngeal supplies only the cricothyroid, yeah. So if you divide your larynx into above the vocal cord and below the vocal cord, below the vocal cord, both sensory and motor is by recurrent laryngeal. Above the vocal cord, the cricothyroid is supplied by the external laryngeal and the sensation is supplied by internal laryngeal. 03:49 Both are coming off the superior laryngeal. You’re right. Now, then you have the pharynx. I’m sorry but do you mind slowing down? Yeah sure. 04:10 Don’t get confused with this, just remember all the muscles in the larynx are supplied by the recurrent laryngeal, except cricothyroid which is supplied by the external division of the superior laryngeal. Okay, that’s it. 04:29 Now, take your sensation below the vocal cord, it’s by the recurrent laryngeal and above the vocal cord it is by the internal division of the superior laryngeal. So that’s it, that’s all they will ask about the larynx. That’s it. Then they might ask you something on the pharynx. What is the pharynx supplied by, mainly? What are the main muscles in your pharynx? Constrictors? Constrictors. So you have your superior constrictor, middle constrictor, inferior constrictor. 05:11 Anything else? Palatoglossals? You’re right. Yeah palatoglossal, styloglossus, stylopharyngeus, those muscles. They are all supplied by the vagus, except the stylopharyngeus. In other words, your larynx, pharynx has to be from vagus with a bit of exception. The glossopharyngeal nerve doesn’t have too many motor branches. It has got the lesser petrosal nerve and a couple of small branches but nothing major. Vagus is a big one. Vagus is the one that mainly supplies most the neck. 05:49 The other way you can remember is you know you have a nasopharynx, oropharynx, and hypopharynx. 06:04 So, nasopharynx, oropharynx, and hypopharynx. We won’t go into detailed anatomy because that is more part like B, but here what you need to remember is your hypopharynx, remember cranial nerve X because it’s lower. Oropharynx is IX and this is V. That means the maxillary division of trigeminal nerve supplies the nasopharynx. So that’s quite easy to remember. If at all you’re asked about nerve supply of the oropharynx, hypopharynx or the nasopharynx. 06:45 So the first one is nasopharynx, oropharynx, hypopharynx and remember V, IX, and X. 06:59 I think I’ll just go through some of the slides now. I know that similar to your upper limb everything is available on the slides so -- In the MCQs they will specifically asked about the triangles of -- Boundaries. Boundaries of the kind of individual triangles that are in the neck or do we just need to grossly be aware of them and not the actual -- You need to be aware of the submandibular triangle and the carotid triangles because they are the most important ones. You don’t have to know about the posterior triangle divisions, but these ones you need to know, because they are anatomically and clinically quite significant. 07:42 So as I said, there’s no new information in these slides, so don’t worry about going through detail. Just to reinforce what we learned. 07:51 We discussed about the hyoid, thyroid cartilage, cricothyroid membrane and then you have the cricoid cartilage. Significance, the larynx and the trachea, does the junction at the cricoid cartilage, and the pharynx with the esophagus. So pharynx begins as the esophagus from C6 vertebra and the trachea is formed from C6 level as well. Right, this is what we went through, so that’s your submandibular triangle, carotid triangle and occipital triangle. Submental triangle, submandibular triangle, carotid triangle, occipital triangle, supraclavicular triangle or the subclavian triangle. 09:04 Theory, you don’t have to read it now. It will be available online. I’m sure you don’t have to know it in detail as long as you have a fair idea of the main muscles, or the only two muscles you need to remember. Well if they say four that will be sternocleidomastoid, trapezius, big triangles, then your digastric and omohyoid. That’s it. 09:37 Triangles and structures in each triangle. Of this, submandibular triangle is very important, remember that, and the carotid triangle, even though there are lots of structures, all you need to remember is carotid sheath. If you remember that, you know that jugular vein, carotid artery, vagus. So if you remember these three, everything else is fine, because these are the three big ones. 10:12 Posterior triangle. All you need to remember is spinal accessory nerve, branches of the cervical plexus. There are these cutaneous ones, brachial plexus and phrenic, but phrenic is quite away from the clavicle here. Carotid artery we don’t have to discuss, the only thing is the bifurcation occurs at the level of C4 and then the branch is the external carotid, exactly what we discussed before. Right, the only one thing that I need to point out here, it’s not very anatomical, but carotid artery stenosis, more than 70% is significant. You need to know the clinical indications. You need to know this amaurosis fugax, at what point you offer surgery to a patient with carotid artery stenosis. So the current guideline say anything between 70 - 99% of stenosis, you need to offer surgery, but 100% stenosis you don’t have to treat. So this is quite important. You may be getting a question in the exam, so if you have a patient with carotid artery stenosis, if it’s 50% of plaque, wait and observe. If it becomes 70% then you get worried. That’s when it’s throwing off embolus. So between 70 and 99 you need to operate, but if it is completely occluded, what do you do? It’s probably throwing off emboli. 11:51 That’s right. But the only thing you need to do is you need to scan the other side. 11:56 Just to make sure that the other side is patent. So if 70 - 99% is asymptomatic, do you still treat? If they are absolutely asymptomatic then perhaps not, but be very careful because they can just have a stroke anytime. They don’t have to have a TIA, they can just have a stroke. So it is better to treat. 12:16 Basically, it’s coming anyway because they have had a symptom or something apparently -- That’s right, yeah but the guideline is 70 - 99%, so in the exam if they ask you say yes. 12:24 Parotid region, branches of the facial nerve, you know that. Parotid gland, parotid ducts and those are your branches. And that is exactly what it supplies. Is it also called Stensen’s duct? The parotid duct, is it also called Stensen’s duct? Stensen’s duct. The submandibular duct is called the Wharton’s duct. Stensen’s duct is 5 cm long. It comes from the anterior border of the submandibular gland, overlies the masseter muscle, pierces the buccinator and empties into the upper second molar tooth. So if you clench your teeth and roll your finger, you’ll feel the parotid duct. On the finger is the parotid duct and that’s the one which pierces the buccinator. Okay, so that’s fine. Branches of the parotid, you know that. We touched upon this when we discussed submandibular gland. So the question might be related to excision of the submandibular gland, lesion or gland. What are the nerves that can be injured? So V1, V2, V3, this is what we said, ophthalmic, maxillary and mandibular. Okay, as per here, the commonest reason for epistaxis is what? Do you mean cause of -- Cause of epistaxis. Usually in the epistaxis, the 90% of it occurs in the Little’s area or the Kiesselbach's plexus. Your question will be related to the arteries in that area. 14:24 Sphenopalatine? Sphenopalatine, yeah. Greater palatine, yeah, very good. Labial, superior labial. Septal arteries? Septal arteries, yeah, and mainly the ethmoidal. Anterior and posterior ethmoidal arteries. 14:42 What is the other significance of the Little’s area apart from -- Infection. Infection! Go on, tell me… It kind of causes cavernous sinus thrombosis because of the relation to the cavernous sinus to get infection. How is the cavernous sinus related to that area? You’re right but -- Is it because of the arterial supply that leads directly to the cavernous sinus? Yes, because whenever you have an arterial supply, the venous drainage will also be going back to that area. In this area, or the Little’s area of the nose, is where your external carotid anastomosis with the internal carotid. Essentially the veins are going back into the cavernous sinus. So you get an infection in this area that leads to cavernous sinus thrombosis, that’s because of this anatomy. So there are not many small arteries you need to know in the face, but these ones are asked, these names. The specific branches of external carotid and internal carotid because of Little’s area, because of epistaxis. 15:49 Right, just one slide for larynx, that’s all you need to know. That’s it. Exactly what we discussed. I’ll leave it to you to remember it. Motor and sensory innervation of the larynx is mainly through two branches of the vagus, superior and recurrent. Superior divides into external, internal. 16:10 External supplies cricothyroid muscle, and recurrent supplies all the muscles in the larynx except cricothyroid. Sensory above the vocal cord is internal laryngeal and below is recurrent. Another question that comes up: Recurrent laryngeal nerve injury, unilateral injury you get hoarse voice, bilateral injury, partial airway obstruction or aphonia. External laryngeal nerve injury, patient’s inability to produce high pitched sounds. So this question will be related to nerve injury or thyroidectomy. Post-thyroidectomy complication will be a question on this. Post-thyroidectomy, patient iss unable to produce high pitched sound and the patient has got hoarse voice, which nerve is injured? And the question would be, unilateral recurrent laryngeal nerve, bilateral recurrent laryngeal, external laryngeal, internal laryngeal. Okay? Pharynx. Nasopharynx. Oropharynx. Laryngopharynx or the hypopharynx. So this what I said: V, IX, X. So remember I said about all your constrictor muscles? Middle constrictor, superior constrictor, inferior constrictor, they are all in that laryngopharynx, right? The laryngopharynx. So that’s why they are all by the vagus. 17:38 Thyroid. The malignancy of thyroid is important, but as far as anatomy is concerned all you need to know is the blood supply of the thyroid. So we discussed about the superior thyroid artery which comes from the external carotid. Then you have the inferior thyroid coming from the thyrocervial trunk, which we’ll cover when we do the thorax, and then you have the thyroid ima artery. So these are the main arteries supplying the thyroid gland. 18:12 So superior thyroid, inferior thyroid, and thyroid ima artery. Thyroidectomy. The only reason for this slide is just to reinforce the idea that you get exactly the same injury in the thyroidectomy and the nerve injuries related to recurrent laryngeal. 18:33 Lymph nodes of the neck. This is what I said, Level I, IA, IB. Level II. Level III. Level IV. The C1, C2 describes the name of lymph nodes. So Level I, level II, level III, level IV, evel V. And the next slide goes through the anatomy of the lymph nodes and what are the areas drained. So this is something you may have to revise quickly before your exam because they might give you a clinical scenario and say, “Which lymph node does it drain to?”
About the Lecture
The lecture Vagus Nerve by Stuart Enoch, PhD is from the course Head and Neck Anatomy—MRCS.
Included Quiz Questions
A 27-year-old male who was recently involved in a car accident was seen by a physician for complaints about his face. On physical exam, miosis, ptosis and anhidrosis were observed. He was diagnosed with Horner’s syndrome, this is caused by injury to an important ganglion. At which cervical level was the ganglion most likely damaged?
- C4
- C2
- C3
- C5
Why is damage to the C4 level, especially dangerous?
- Birfucation of the carotid arteries
- Birfucation of the femoral arteries
- CVA
- Posterior scalenes
Which of the following structures comprises the infrahyoid strap muscles?
- Sternohyoid, sternothyroid, thyrohyoid and omohyoid muscles
- Sternohyoid, sterncladomastoid, thyroid and scalene
- Anterior scalene, sternothyroid, thyrohyoid and omohyoid
- Posterior scalene, pectoral , thyrohyoid and omohyoid
A 55-year-old female came into the ER complaining of intense jaw pain and bloody saliva trickling from her mouth. She complained of her tongue “not feeling normal”. A diagnosis of fractured mandible was made. Which of the following problems could be caused by a lesion in the nerve fibers entering the mandible?
- Altered general sensation of the anterior 2/3 of the tongue
- Altered general sensation of the posterior 1/3 of the tongue
- Altered taste of the anterior 1/3 of the tongue
- Altered taste of the posterior 2/3 of the tongue
Which one of the following is found in the occipital triangle?
- Lymph nodes and spinal accessory nerve
- Internal jugular vein and lymph nodes
- External jugular vein and phrenic nerve
- Lymph nodes and aorta
An 18-year-old male was bitten by a bear while camping. He was injured around the lower edge of the right clavicle to the shoulder. Which of the following structures is most likely to be damaged in this area, which is also known as the supraclavicular triangle?
- Subclavian artery, brachial plexus, subclavian vein
- Aorta, thoracic duct, subclavian vein
- Thoracic duct, subclavian artery, brachial plexus
- Thoracic duct, subclavian vein, subclavian artery
A patient diagnosed with metastatic neck carcinoma is scheduled for a radical neck dissection. This operation encompasses removal of which of the following structures?
- Ipsilateral neck lymph nodes, spinal accessory nerve, internal jugular vein, sternocleidomastoid muscle
- Contralateral neck lymph nodes, spinal accessory nerve, internal jugular vein, sternocleidomastoid muscle
- Only affected lymph nodes, spinal accessory vein, internal jugular vein, sternocleidomastoid muscle
- Spinal accessory nerve, internal jugular vein, sternocleidomastoid muscle, external jugular vein
A 25-year-old female was evaluated in the ER for persistent numbness on the right side of her face and jaw. X-ray imaging failed to show abnormalities, but upon further MRI testing a schwannoma was found. This led to compression of a nerve which exits the skull. Which of the following foramina does this nerve exit from?
- Foramen ovale
- Foramen orbital
- Foramen spinosum
- Foramen rotundum
A patient complains of abnormal eye sensation and movement. The doctor administers a special test in which he uses a cotton Q-tip to test the blink reflex by touching the cornea. The patient doesn’t blink in response to stimulation. Which cranial nerve is most likely affected?
- V1 of trigeminal nerve
- V2 of cranial nerve V
- cranial nerve II
- cranial nerve III
Which of the following cranial nerves is responsible for abduction of the eye?
- Cranial nerve VI
- Cranial nerve V
- Cranial nerve III
- Cranial nerve XII
Which of the following structures pass through the Superior Orbital Fissure?
- Cranial Nerves III, IV, V1 branch, VI
- Cranial Nerves II, III, IV
- Cranial Nerves IV, V2 branch, VI, VII
- Cranial Nerves III, IV, VI, VII
Which of the following glands is NOT innervated by the parasympathetic fibers of cranial nerve VII?
- Parotid gland
- Lacrimal gland
- Sublingual gland
- Submandibular gland
Which of the following is NOT supplied by branches of the trigeminal nerve?
- Taste sensation of the tongue
- Cornea
- Anterior sensation to ⅔ of the tongue
- Nares
A 60-year-old smoker presents with a painless, swollen superficial lobe of a gland in his mouth. Biospy reveals the presence of a Warthin tumor posterior to the mandible. Which of the following glands was the tumor most likely biopsied from?
- Parotid Gland
- Sublingual gland
- Submandibular gland
- Optic gland
Which of the following consists of the branches of the facial nerve?
- Temporal, Zygomatic, Buccal, Mandibular, Cervical
- Optic, Zygomatic, Buccal, Cervical
- Temporal, Zygomatic, Buccal, Optic, Cervical
- Temporal, Zygomatic, Sternocleidomastoid, Mandibular, Cervical
Which of the following in NOT supplied by the external carotid artery?
- Anterior auricular artery
- Superior thyroid artery
- Lingual artery
- Facial artery
Which of the following provides motor supply to the diaphragm?
- Phrenic nerve
- Intercostal nerve
- Recurrent laryngeal nerve
- Thorax nerve
Which of the following is located in the anterior triangle of the neck?
- Vagus nerve
- Trochlear nerve
- External jugular vein
- Acessory nerve
A 50-year-old male undergoes an endarterectomy of the internal carotid artery. Unfortunately a nerve was lacerated during dissection which has affected his ability to speak. Which of the following nerves was most likely damaged?
- Hypoglossal nerve
- Largyngeal nerve
- Lingual nerve
- Phrenic nerve
Two weeks following a thyroidectomy, a patient complains of hoarseness and inability to speak like she used to. Which branch of the vagus nerve was most likely affected given the patient’s symptoms?
- Recurrent Laryngeal nerve
- Lingual nerve
- Phrenic nerve
- Glossopharyngeal nerve
Level 1 lymph nodes are anterior to which of the following anatomical landmarks?
- 2, 3, 4 uppper jugular middle and lower jugular between hyoid and thyroid cartilage
- Hyoid bone
- Omohyoid bone
- Mastoid bone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Clear and precise information on important structures of neck. Easy to remember!