Playlist
Show Playlist
Hide Playlist
Urinary Tract Infections (UTI, Bladder Infection) in Children: Pathology & Diagnosis
-
Slides UTI Pediatrics.pdf
-
Download Lecture Overview
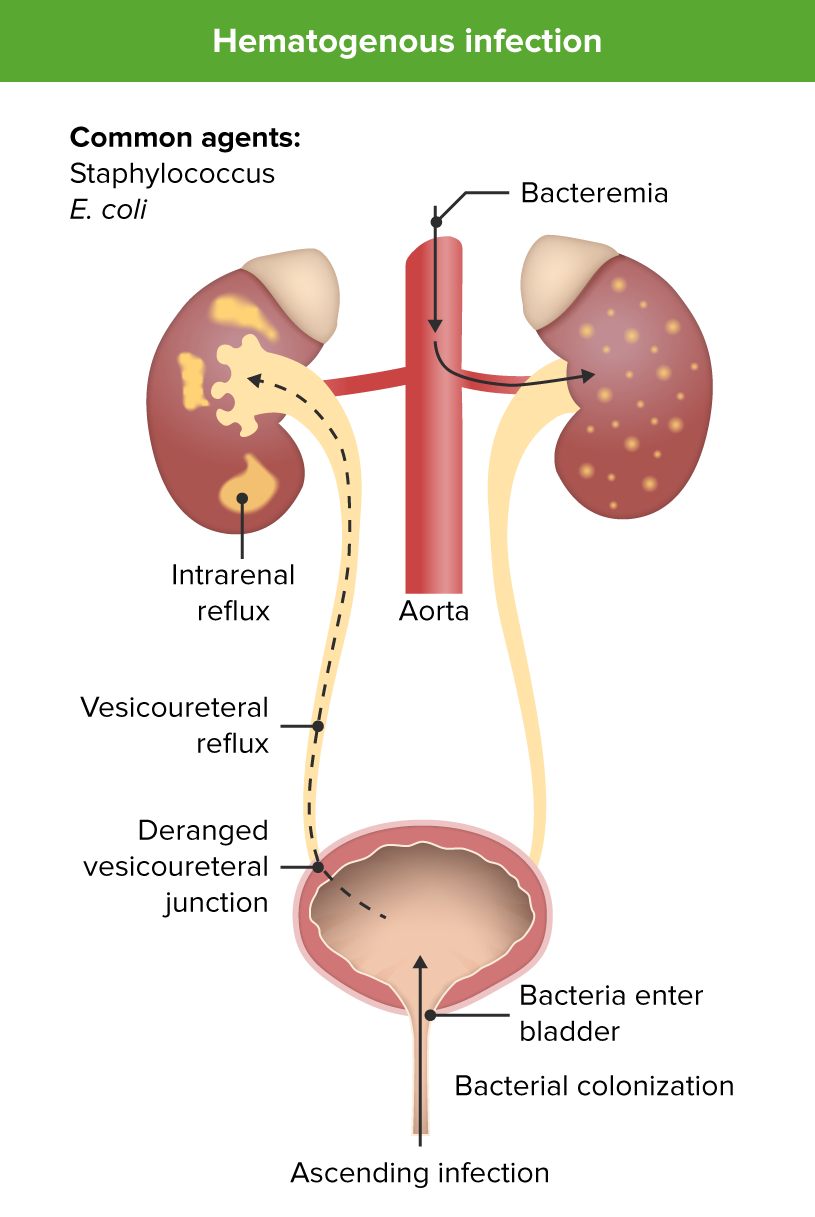
00:00 In this lecture, we're going to review Urinary Tract Infections in Children. A urinary tract infection is an infection by bacteria of the bladder which is cystitis or the kidney which is pyelonephritis. The site of infection is harder to tell clinically in infants because they have a nonfocal exam. Older children will complain about pain while peeing, but it’ll be generally suprapubic in cystitis or they’ll have pain over their costovertebral angle to palpation when they have a pyelonephritis. About 7% of infants who have a fever have a urinary tract infection. 00:43 That’s generally speaking under, say, a year of age. The problem is is that our gold standard for testing for urinary tract infection, which is the urine culture, 1% of asymptomatic infants and adolescents will have bacteria in their urine, will have an abnormal urine culture, so the problem is if we see a febrile infant or adolescent and we’re suspecting urinary tract infection but we’re not sure, there is a 1% false positive rate. The most likely organism in a urinary tract infection is <i>E. col</i>i and that accounts for about 80% of urinary tract infections but there are are others that can pop up including <i>Klebsiella, Proteus, Citrobacter, Enterobacter,</i> <i>Enterococcus,</i> and <i>Enterococcus</i> is important because it’s resistant to many of the antibiotics that we might choose for a UTI, <i>Staphylococcus</i>, very rare and in particular it could be <i>Staph saprophyticus</i>, and <i>Pseudomonas</i>. So, what are the risk factors for infants and children getting urinary tract infection? The one that’s often missed is constipation. Constipation is really common in children and infants with urinary tract infections and managing constipation is critical to prevention of further urinary tract infections. Children with a history of vesicoureteral reflux or any other underlying nephropathy are at increased risk for urinary tract infections. This includes patients with horseshoe kidney, patients with ureteropelvic junction problems or posterior urethral valves. All of these things put children at increased risk for UTI. Patients with dysfunctional voiding such as the neurogenic bladder are at increased risk for UTI. So, for example, a patient with spina bifida who has to self cath is at very significant increased risk. Young children are at higher risk than older children. In particular, less than a month, it’s very common; under a year, it’s still very common but it gets less common as they age. Any girl after about 3 months of age is at increased risk over a boy for having a urinary tract infection. The penis provides some sort of protective capacity. In children under 3 months of age, because oftentimes urinary tract infections are pyelonephritis, which is spread through bacterial spread of the bacteria, in fact males are slightly more likely to have UTI very early in infancy than females. So this really doesn’t cross over until about 3 months of age. In adolescents, especially adolescent girls, sexual activity increases risk of urinary tract infection. So, here are the 2 methods by which children are most likely to get a urinary tract infection. There is bacteremia that then lands in the kidney and causes a pyelonephritis and that tract infection descends downward, that's more common in infants and then there is ascending urinary tract infections. Most people at some point are bacteruiric, they get a little bit of bacteria in their bladder. Those bacteria are continuously flushed out through the process of urination. Occasionally, those bacteria can ascend upwards through the urethra and the ureter and up into the kidney, so an ascending infection is also possible. In general, in infants under 2 years of age, they will present with relatively nonspecific findings: fever, irritability, and poor feeding, sometimes vomiting. Over 2 years of age, you’re more likely to get a good story for it. They’ll have the fever but they may have CVA tenderness or bladder tenderness. They may complain of dysuria and they often have urgency or incontinence. So, if we suspect a urinary tract infection, it’s important to collect some urine. There are several different techniques we can use. In children who can pee on command, we can do a clean catch where we have them clean themselves off, pee a little bit on the toilet and put the rest in the cup. That’s very effective. For younger children, we may choose to do a bag urine. The problem with bag urine is there is a higher false positive rate. So, patients may have some contamination in that bag of a little fecal material, which will look like a urinary tract infection. However, if the bag urine is negative, you can assume that the child does not have a urinary tract infection. Catheterized urine is probably the way to go in these younger children in that when you catheterize them, you can get a cleaner specimen and you're less likely to have a false positive. In catheterized urine, we then go and insert a catheter into the urethra of the patient and up into the bladder and collect the urine. Of course, it’s sterilized first. Catheterized urine is appropriate to send for culture although bag urine generally not. 05:51 Another more invasive way one could collect urine is through a suprapubic tap or aspiration. 05:57 This is when a needle is introduced directly through the abdominal wall generally slightly angling downward just over the pubic symphysis. This is generally a fairly effective way and in experienced hands, you usually get a result. There’s not much risk for perforation of a viscus because you’re going directly into the bladder. However, this is a very painful experience and generally we prefer to do catheterized sampling. The urinalysis is a very effective test for a urinary tract infection. It is in fact 98% sensitive. However, it’s only 65% specific. That means it has about a 35% fall positive rate. A urinalysis has a likelihood of showing you when you have a urinary tract infection a positive result but when you don’t, it has a reasonable shot of still showing you a positive result. The elements of the urinalysis that indicate whether a patient have a urinary tract infection include white count, red count, leuk esterase, and nitrites. 07:00 The presence of nitrites in a urinalysis is strongly associated with bacterial presence in the urine, but this doesn't necessarily indicate a urinary tract infection (UTI). This finding may represent asymptomatic bacteriuria. 07:16 For pediatric patients, we typically look for both positive white blood cells (WBCs) and leukocyte esterase in addition to nitrites to support a UTI diagnosis. 07:28 Finding isolated positive nitrites without these other markers should raise suspicion for a false positive result, though this pattern can occasionally occur in true infections. 07:40 So, let’s say that we have a urinalysis and we suspect the patient has a UTI, what is the gold standard? Well, the gold standard is culture but remember the culture is not that golden. By that I mean that many patients, 1%, will have a false positive urinary tract infection culture because they have asymptomatic bacteriuria and there’s something else going on. For a suprapubic tap, we recommend that any bacteria counts as a positive urine culture. 08:14 For catheterized urine specimens, we recommend using 10,000 colony-forming units per milliliter as the threshold for a positive culture. 08:24 While the previous American Academy of Pediatrics guideline suggested 50,000 CFU/mL, recent evidence indicates that lowering the threshold to 10,000 CFU/mL improves sensitivity without significantly reducing specificity. 08:41 As a result, many clinicians now use this lower cutoff value for diagnosing UTIs from catheterized specimens. 08:49 There’s not a lot of evidence for that 10,000-50,000 range in terms of whether these are likely to be positives or negatives and it is difficult to determine because of asymptomatic bacteriuria and not having a really clear gold standard. That said, you can either use 10,000 or 50,000 as your cut off for a catheter specimen. Generally, for a clean catch, we use 100,000. These are rough estimates. Remember, there is no real gold standard here and many times we’ll just use our clinical suspicion in combination with these data. What’s key is you should not obtain a bag urine to check for a culture because of the false positive rate and remember there’s no blood test that is diagnostic of a UTI. There is no role for getting a CBC when you’re trying to rule out a urinary tract infection.
About the Lecture
The lecture Urinary Tract Infections (UTI, Bladder Infection) in Children: Pathology & Diagnosis by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of Urinary Tract Infections
- Diagnosis of Urinary Tract Infections
Included Quiz Questions
Which of the following elements of a urinalysis is most SPECIFIC for urinary tract infection in children?
- Positive urinary nitrites
- Elevated urine WBCs
- Elevated urine RBCs
- Elevated urine leukocyte esterase
- Positive urine glucose
Which of the following is NOT a common bacterial pathogen found in pediatric urinary tract infections?
- Haemophilus influenzae
- Citrobacter
- Proteus
- E. coli
- Klebsiella
Which of the following is NOT a common risk factor for urinary tract infections in children?
- Diarrhea
- History of vesicoureteral reflux
- Constipation
- Dysfunctional voiding
- Sexual activity in adolescents
Which of the following statements are FALSE regarding urinary tract infection?
- Urinalysis is specific but not very sensitive
- Elements of urine analysis include WBC count, RBC count, leukocyte esterase and nitrites.
- Children less than 2 years of age with a UTI can present with irritability, fever and poor feeding.
- A catheterized urine sample is more suited for culture than a bag sample of urine.
- Nitrites are very specific for UTI.
Which of the following is considered the gold standard for testing in patients with a suspected urinary tract infection?
- Urine culture on catheterized sample
- Urinalysis on clean catch sample
- Urinalysis on urinary bag sample
- Urinalysis from suprapubic tap sample
- Culture on a urinary bag sample
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture as usual. However, I would have liked to see the different sensitivities and specifities per analysis (leuco-esterase, blood, etc.) and altogether (leuco+blood, etc.) as can be found in Nelson's or other sources. All in all, I learned new things, thanks!