Playlist
Show Playlist
Hide Playlist
Nephrolithiasis (Kidney Stones): Uric Acid
-
Slides Nephrolithiasis RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
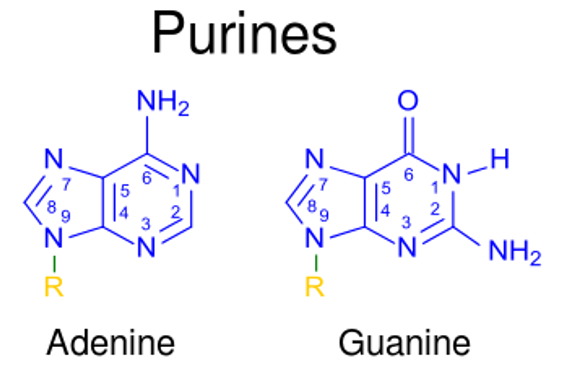
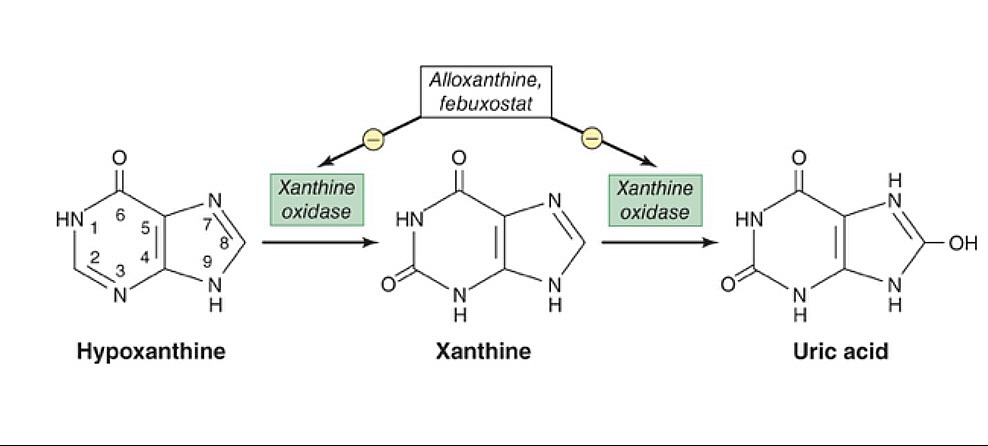
00:00 Let’s go into other types of stones, shall we? This is a uric acid, so think about as to where you get uric acid. 00:06 Be careful not to get this confused with urea, one has nothing to do with the other. 00:11 Uric acid, a breakdown of your purines which only means it’s a breakdown of DNA, which only means it comes from cells. 00:18 Are we okay or are you producing too much uric acid? What else may cause this? Well, cancer, chemotherapy is a big deal and with chemotherapy, you’re breaking down lots and lots, and lots of cancer cells, cancer cells of course contain DNA, and so therefore, you’re releasing all this DNA into circulation, you may then be introducing what? Good, uric acid is of course referred to, take a look at the notes here. 00:42 We have tumor lysis syndrome. 00:45 Are we clear? Alright, so here, as the name applies, uric acid, decreased pH, here, things get a little different. 00:52 This crystal that you’re going to find is going to be rhomboid or rosette and the crystal that’s rather on x-ray will be radiolucent, on CT, minimally visible because it’s lucent. 01:07 The first stone now that we’re seeing in which its characteristics are clear on ultrasound, U/S stands for ultrasound, may also be visible. 01:16 In other words, factors include, we talked about this dehydration, I told you about during let’s say holidays, not consuming as much proper hydration, maybe drinking too much alcohol perhaps, and then may result in precipitation. 01:31 What else? Climate, acidic pH, hyperuricemia we talked about tumor lysis syndrome. 01:36 What do you wanna do here with the urine? You want to alkalinize it or maybe not even produce the uric acid to begin with. 01:46 Now, we come into cystine. 01:47 With the cystine stone, it’s rather interesting. 01:49 We talked about this back in nephrology a little bit where we referred to different reabsorption issues and I gave you the pneumonic COLA. 01:59 If that worked for you, cystine, ornithine, lysine, arginine, and I want you to focus upon cystine. 02:04 A hexagonal crystal, clear. 02:06 So with that said, we have now a cystine decreased pH in your urine. 02:11 X-ray will be radiolucent and sometimes visible on CT. 02:15 You’re not able to properly take in your cystine. 02:18 It’s autosome recessive disease, genetic, in the PCT, you’re not able to properly take up there your amino acids, cystine, ornithine, lysine, arginine, and these may then form staghorn, so be careful with that term staghorn. 02:33 All staghorn means is a huge stone actually but take a look at the picture here. 02:37 That looks rather large. 02:38 It could actually be confused by a layman or if you’re not paying attention on gross examination as being a staghorn, meaning, what? Oh, maybe magnesium ammonia phosphate, but it’s impossible if the urine was pH and it was decreased as for uric acid. 02:55 And if you’re thinking about cystine, a decreased pH, here you go. 03:01 And then if it’s staghorn in dealing with magnesium ammonia phosphate, its pH will be increased.
About the Lecture
The lecture Nephrolithiasis (Kidney Stones): Uric Acid by Carlo Raj, MD is from the course Nephrolithiasis.
Included Quiz Questions
Which of the following is generally required for the definite treatment of staghorn magnesium-ammonium-phosphate stones?
- Surgery
- Diuretic therapy
- Antibiotics
- Thiazides
- Low sodium diet
Which stone type is NOT visible by radiograph?
- Uric acid
- Calcium oxalate
- Struvite
- Magnesium-ammonium-phosphate
- Calcium phosphate
What is the typical shape of uric acid crystals under light microscopy of urine?
- Rhomboid
- Hexagonal
- Envelope
- Dumbbell
- Coffin lid
Which of the following is NOT a risk factor for uric acid stones?
- Alkaline urine
- Decreased urine volume
- Tumor lysis syndrome
- Hyperuricemia
- Arid climate
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good presentation and good pronunciation for being foreign. Thanks for the difference between urea and uric acid.
Ugly way of explaining. Weird pronounciation. Not so clear explanation.